JAMA子刊:COVID-19高烧患者更易发展为ARDS,甲基强的松龙治疗或可降低死亡率
2020-03-17 王芳 生物探索
急性呼吸窘迫综合征(ARDS)是COVID-19患者的主要死因。不过,目前尚不清楚哪些人群更易发展为ARDS,以及患者从ARDS发展到死亡与哪些因素相关。
急性呼吸窘迫综合征(ARDS)是COVID-19患者的主要死因。不过,目前尚不清楚哪些人群更易发展为ARDS,以及患者从ARDS发展到死亡与哪些因素相关。
3月13日,中国多所医院的研究人员联合发布在《JAMA Internal Medicine》的一项涵盖201名COVID-19确诊患者的研究报告揭示了与这两个过程有关的因素,并提出,免疫激活可能是患者发展为ARDS的重要原因,但是免疫反应较弱可能导致老年人死亡风险更高,甲基强的松龙治疗或能用于挽救患者的生命。
这些患者于2019年12月25日至2020年1月26日被收治在武汉市金银潭医院,中位年龄为51岁(IQR,43-60岁),其中男性患者占比为63.7%。截至2020年2月13日,144名患者(71.6%)已出院,住院中位时间为13天,另有13名患者仍在住院。
患者从入院到发展为ARDS的中位时间为2天(IQR,1-4天)。治疗期间,84名患者发展为ARDS,其中67人接受了机械通气,最终有44人死亡。在死亡患者中,38人(86.4%)接受了无创机械通气,5人(11.4%)接受了有创机械通气,1人(2.3%)接受了体外膜氧合。
研究人员发现,与无ARDS的患者相比,那些发展为ARDS的患者往往具有以下特征:老年人(≥65岁),就诊时有高烧症状(≥39℃),患有高血压、糖尿病等合并症,中性粒细胞增多,淋巴细胞减少,终末器官相关指数、炎症相关指标和凝血功能相关指标升高。另外,接受类固醇药物甲基强的松龙(具有消炎及抗过敏作用)治疗的患者也更有可能发展为ARDS。
尽管中性粒细胞的增多可能造成中性粒细胞的活化,从而对病毒产生免疫反应,但这也可能会导致“炎症风暴”(细胞因子风暴),使患者出现发热、疲劳等症状。已有研究表明,细胞因子风暴是导致ARDS的重要原因。这或许能够部分解释为什么有高热症状的患者更容易发展为ARDS。不过,尽管高热与发生ARDS的可能性较高有关(HR,1.77;95%CI,1.11-2.84),但是却与死亡呈负相关(HR,0.41;95%CI,0.21-0.82)。
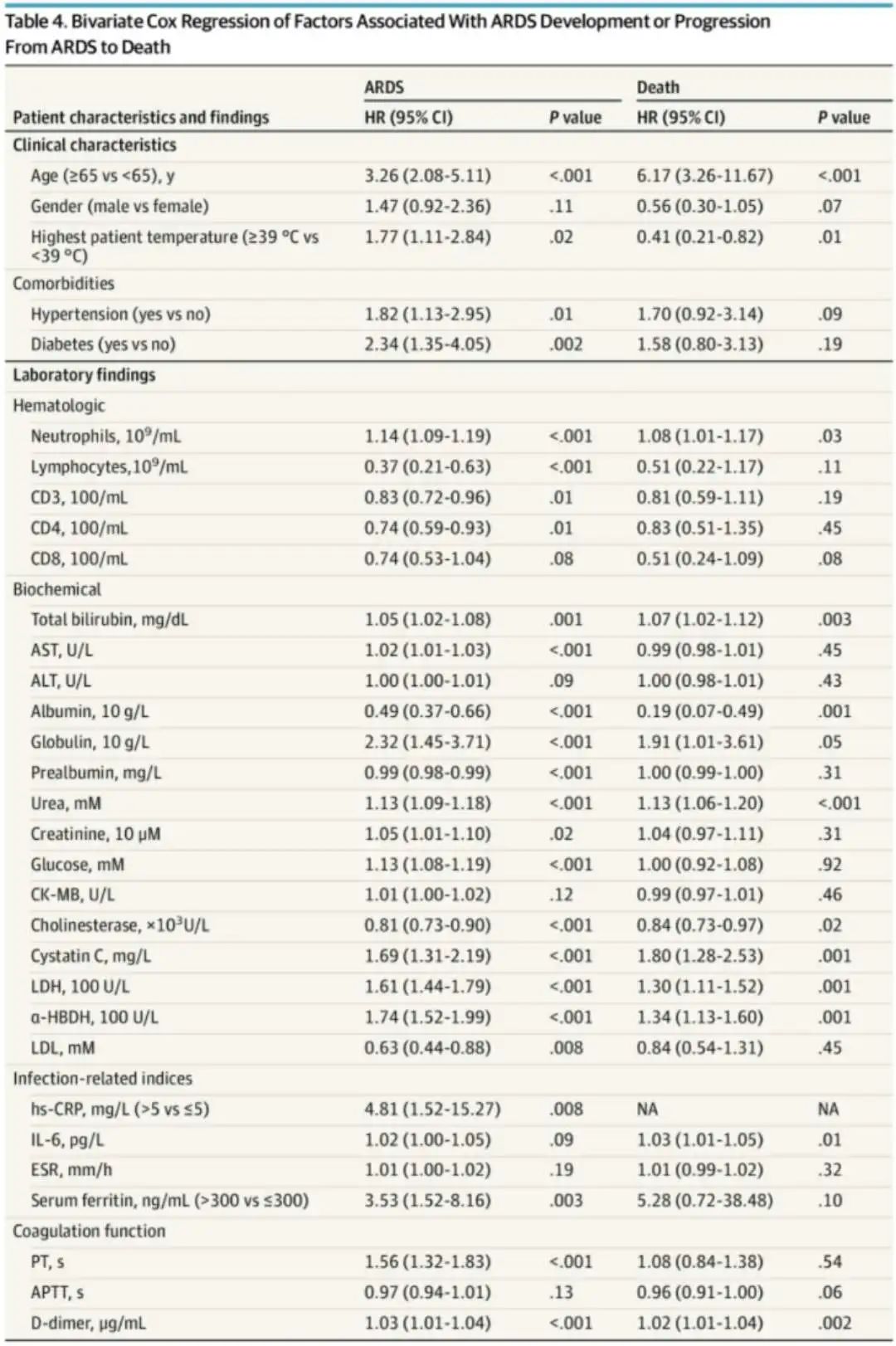
与ARDS发展或从ARDS发展到死亡相关的因素的双变量Cox回归
进一步分析ARDS死亡病例发现,与存活患者相比,死亡患者的年龄更大(差值为18岁,95%CI为13.0-23.0)。另外,死亡的患者患有高血压的比例更高,接受抗病毒治疗的可能性更小,同时他们的肝损害指数、肾功能不全指数、炎症相关指数、凝血功能指数均显著升高,淋巴细胞计数以及CD8 T细胞显著减少。
尽管此前有学者不建议在治疗中使用皮质类固醇激素,认为这可能会加重与COVID-19相关的肺损伤,但是这项研究表明,类固醇药物甲基强的松龙似乎降低了ARDS患者的死亡风险。在发展为ARDS的84名患者中,50名接受了甲基强的松龙治疗的患者里有23例死亡(46.0%),而34名未接受甲基强的松龙治疗的患者里有21例(61.8%)死亡。
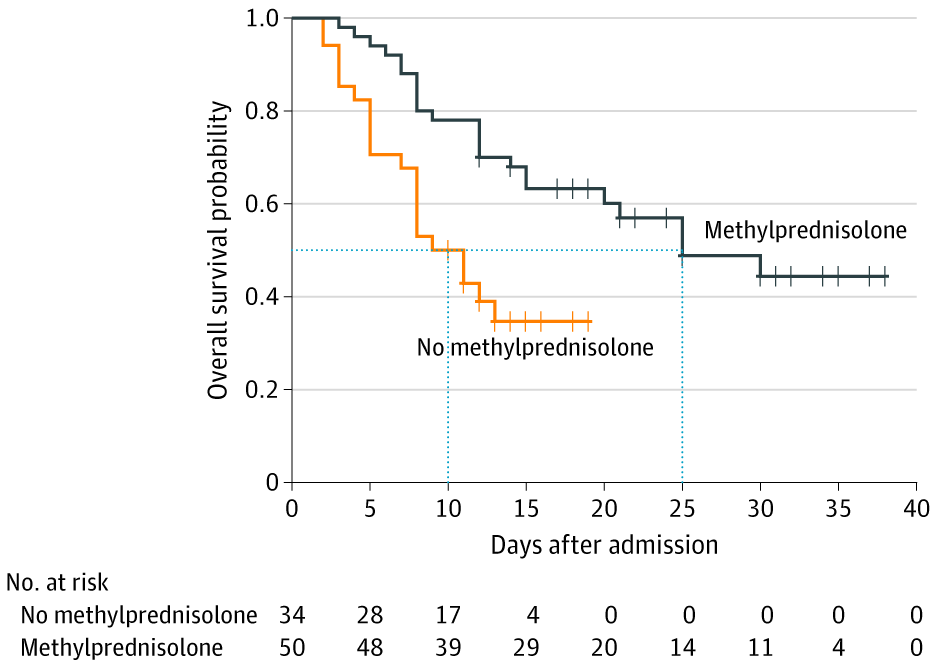
接受和未接受甲基强的松龙治疗的ARDS患者的生存曲线
《柳叶刀》最新在线文章也提出,从过去的试验数据来看,在过度炎症中,免疫抑制可能对COVID-19患者是有益的,使用皮质类固醇激素或许能够帮助过度炎症患者提高生存率。
目前,中国以外地区COVID-19确诊病例数已经超过8万例。这项研究或许能够帮助其他国家和地区的医护人员更好地应对疫情,降低因ARDS造成的死亡。
原始出处:
Chaomin Wu,et al. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA. March 13, 2020
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言











#ARDS#好文
95
#强的松#
60
#甲基强的松龙治疗#
67
#RDS#
83
#甲基强的松龙#
73
顶刊就是顶刊,谢谢williamhill asia 带来这么高水平的研究报道,williamhill asia 科里同事经常看williamhill asia ,分享williamhill asia 上的信息
74