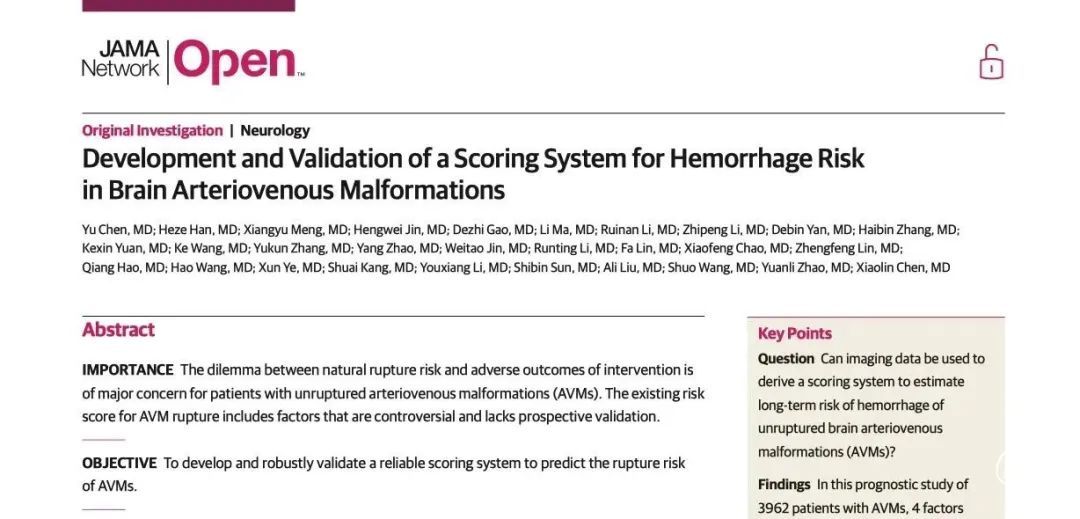
Neurology:腔内活检术可获得脑动静脉畸形(bAVM)分子图谱、识别潜在基因表达信号异常,或有助于实现精准医学治疗!
2022-03-12 Naomi MedSci原创
近日,研究人员通过对脑动静脉畸形患者行腔内活检,利用下一代RNA测序对bAVMs进分子图谱分析,识别治疗靶向途径,并从活体患者中未破裂的bAVM推断出流式介导的转录改变,可能有助于促进bAVM精准治疗
脑动静脉畸形(bAVMs) 是一种在动脉和静脉间形成直接连接血管缠结的脑血管畸形。部分bAVM的会导致脑出血,这也是年轻人脑出血的主要原因。然而,大多数bAVM并发生不出血。随机对照试验表明,介入治疗如血管内栓塞、立体定向放射外科或手术切除死亡率和卒中发生率更高,治疗方法仍然存在争议。
精确医学使临床医学发生了革命性的变化——最显著的是在肿瘤学方面。大多数动静脉畸形的发生没有明确的遗传原因(>95%),但是最近新的测序工作发现了ras-MAPK信号通路中的体细胞激活突变,如在大多数的散发性bAVM中的原癌基因KRAS和BRAF。有针对性地抑制ras-MAPK通路可以逆转实验模型中的bAVM病理,并正在颅外血管畸形中进行试验。尽管如此,还是有针对性地抑制ras-MAPK通路可以逆转实验模型中的bAVM病理,并在颅外血管畸形中进行试验。因此,分子图谱仅适用于开放手术切除的血管畸形。这里有几个局限性:(1)获得的信息对临床决策的影响很小;(2)由bAVM的分子特征指导的精确药物治疗是不可能的;(3)没有分子信息可以从非手术切除的血管畸形中获得。因此,目前还没有从活体患者的人类脑血管病变中提取分子信息的方法。
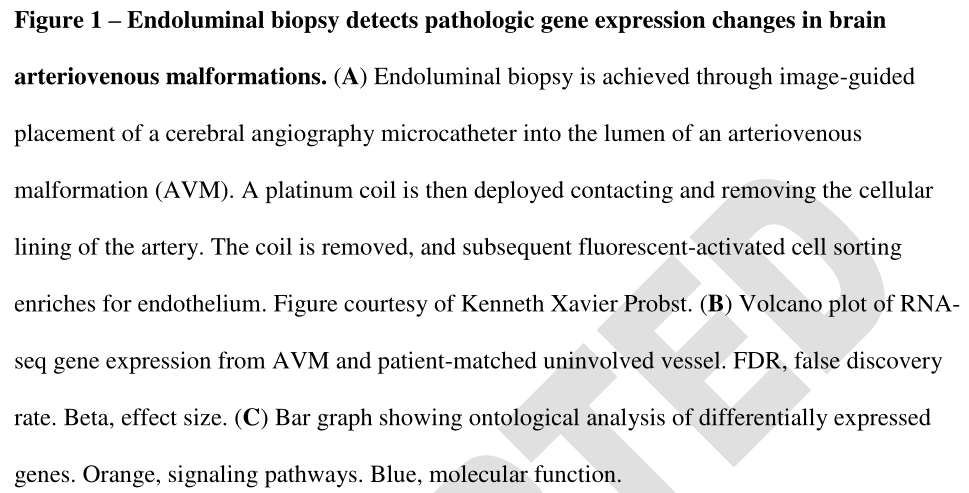
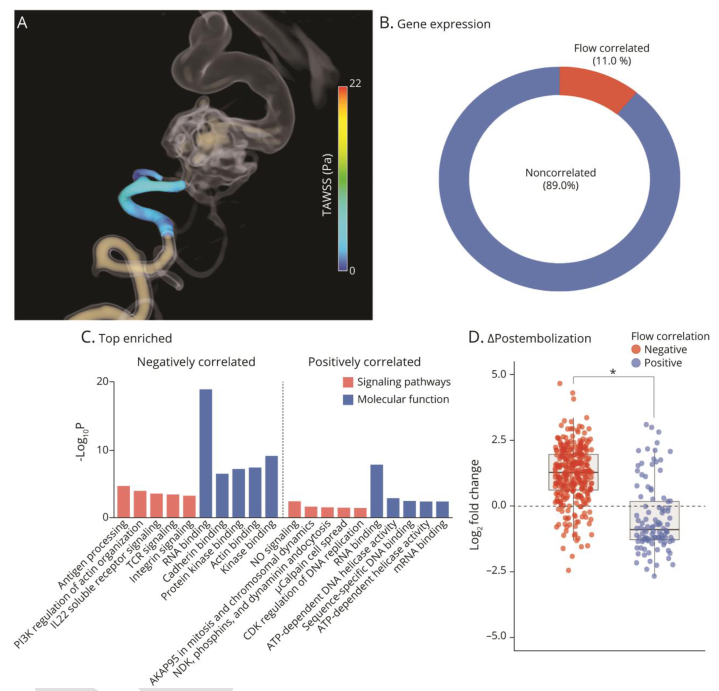
为了解决人类脑血管精确医学翻译的这一障碍,一项发表在Neurology的研究试图使用脑血管造影术的诊断金标准,即从脑血管系统内取样血管腔的细胞,展示了脑血管造影引导的腔内活检的可行性和准确性,利用下一代RNA测序(RNAseq)对bAVMs进行分子图谱分析,识别治疗靶向途径,并从活体患者中未破裂的bAVM推断出流式介导的转录改变。
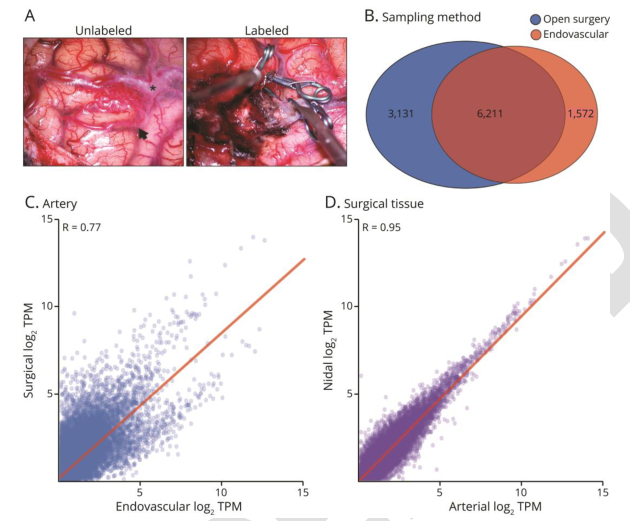
研究人员对成人未破裂型脑动静脉畸形患者行腔内活检和计算流体动力学模拟(CFD)。每个患者都接受了手术切除,并从毗连的动脉节段取样细胞。荧光辅助细胞对在Illumina HiSeq4000测序仪上测序的浓缩内皮细胞进行分选。RNA测序(RNAseq)定量检测基因表达。进行差异基因表达、本体论及相关分析。用定量逆转录聚合酶链反应(RT-qPCR)对结果进行验证。
- 研究共纳入4例患者行腔内活检,无并发症。
- 腔内活检每例获得269.0±79.9个细胞(对照组:309.2±86.6cells;bAVM:228.8±133.4)。
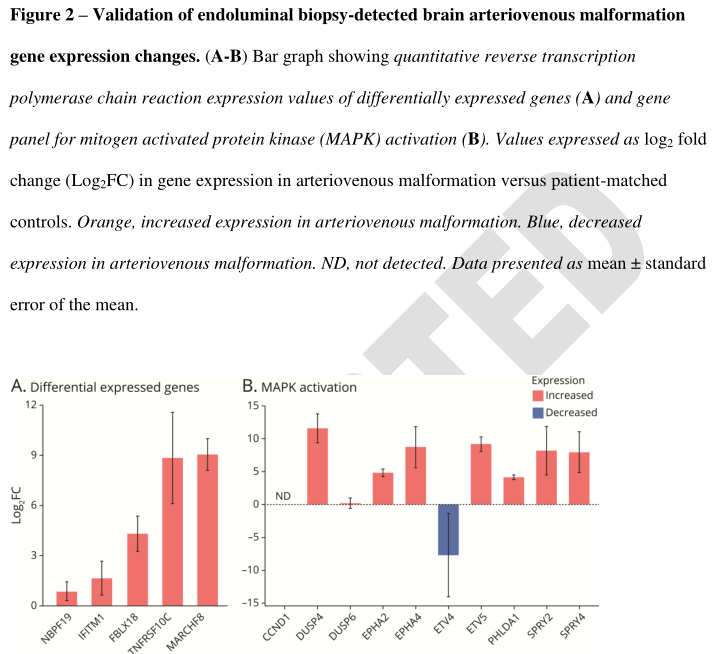
- RNAseq在bAVM中鉴定出106个差异表达基因(DEG)(FDR0.0 5)。
- DEG富集了包括RAS-MAPK信号在内的bAVM致病级联反应(p<0.05),并通过RT-qPCR和MAPK/细胞外信号调节激酶(MEK)抑制剂反应的小组预测得到证实。
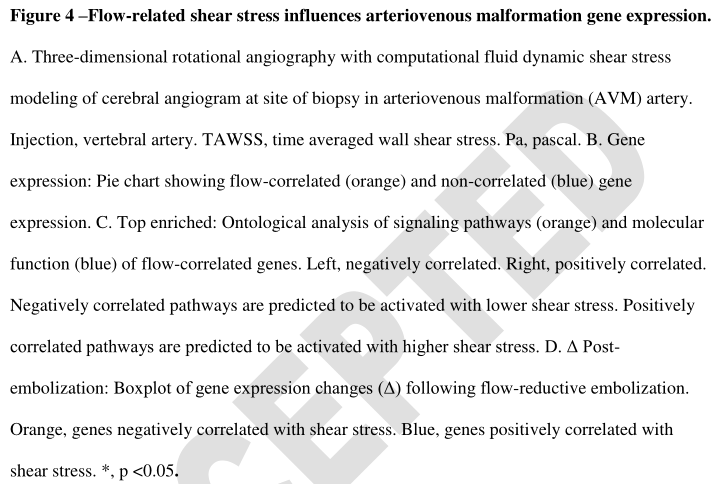
- 与患者匹配的手术切除组织相比,腔内活检检测到83.3%的基因和全基因组表达强烈相关(Pearson r=0.77)。
- CFD测量的壁面切应力与炎症途径上调相关。
- 栓塞前后样本的比较证实了血流介导的基因表达变化。
EB可获得活体患者的bAVM的分子图谱。基因表达谱类似于开放手术获得的组织,并识别bAVM中潜在的靶向RAS-MAPK信号异常。与CFD结合可以确定流介导的转录改变。腔内活组织检查可能有助于促进对人类bAVM的精确医学方法的试验。
缩写:bAVM,脑动静脉畸形;MAPK,丝裂原激活激酶;CFD,计算流体动力学模型;degs,差异表达基因;TPM,百万转录本;MEK,MAPK/细胞外信号调节激酶。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言
















#动静脉畸形#
90
#AVM#
64
#分子图谱#
91
#Neurol#
92
#静脉#
86
#活检#
69
#基因表达#
114
#畸形#
67
#精准#
95