Neurology:卒中相关性血脑屏障渗漏一例
2021-12-15 ANDs 网络
FLAIR序列上与卒中相关的蛛网膜下腔和眼部钆渗漏可能代表了血脑/眼屏障破坏。早期的一份报告描述了卒中后>1个月进行的MRI可见到PVS钆渗漏。类淋巴系统(glymphatic)(在脑脊液-间质液交换
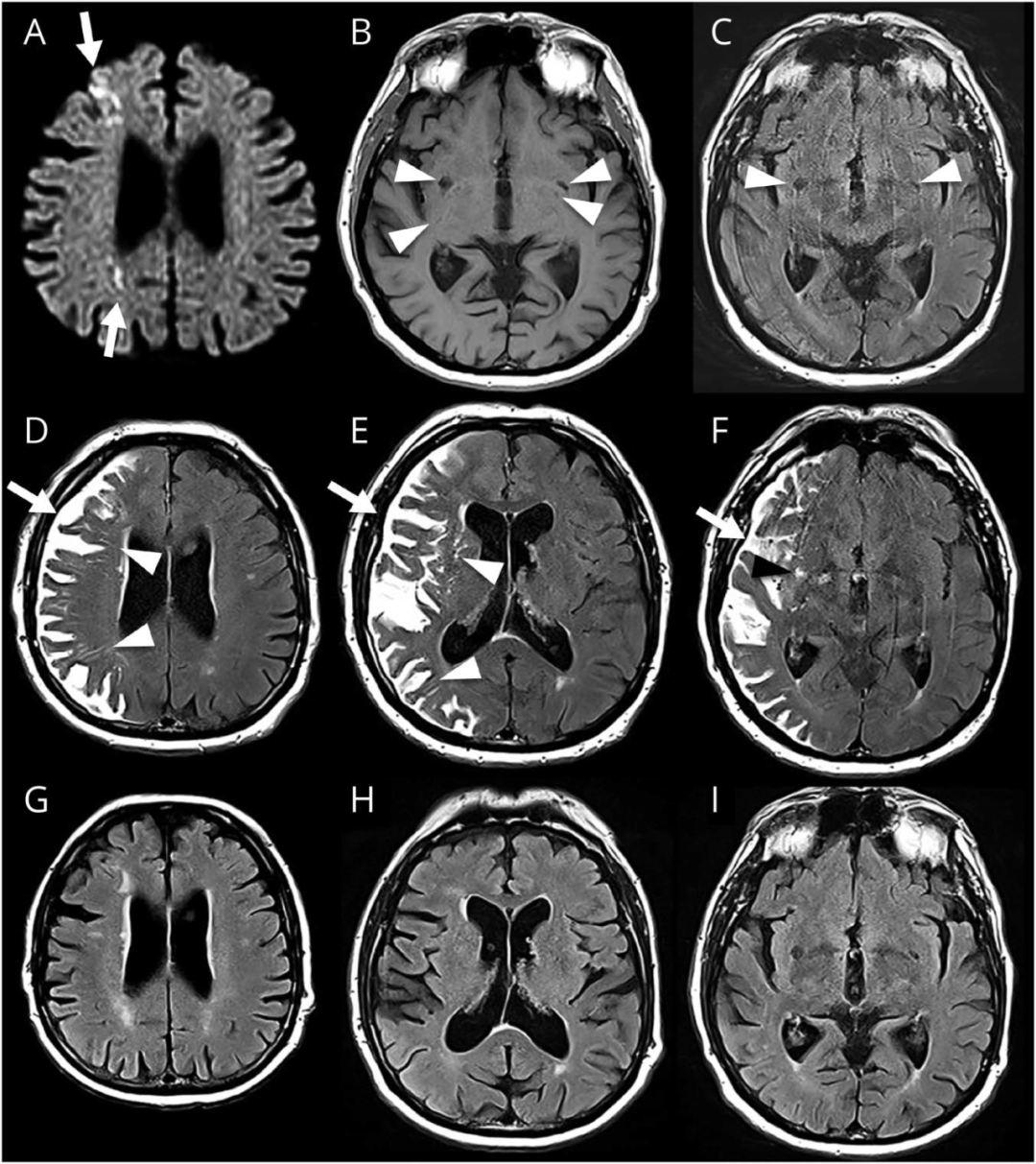
74岁,男性,右侧分水岭梗死。
入院时钆增强MRI显示右侧分水岭梗死(下图)。肾功能正常。4小时后MRI显示同侧血管周围间隙(PVS)和蛛网膜下腔FLAIR高信号,可能与卒中相关性延迟性钆渗漏有关(图)。10天后的MRI显示蛛网膜下腔/血管周围异常完全消失(图)。
下图,入院MRI(钆注射 MRA)显示右侧梗死(A,DWI)和血管周围间隙(PVS)(B,T1加权成像;C,FLAIR)。(D–F)四小时后,MRI显示同侧蛛网膜下腔(箭头)和深部及皮质下PVS(箭头)FLAIR高信号,为钆渗漏所致。(G–I)10天后观察到蛛网膜下腔/血管周围FLAIR异常信号完全消失:
FLAIR序列上与卒中相关的蛛网膜下腔和眼部钆渗漏可能代表了血脑/眼屏障破坏。早期的一份报告描述了卒中后>1个月进行的MRI可见到PVS钆渗漏。类淋巴系统(glymphatic)(在脑脊液-间质液交换中发挥作用)可能参与了蛛网膜下腔和PVS中观察到的卒中相关性血脑屏障渗漏。
文献出处:
Perivascular and Subarachnoid Fluid-Attenuated Inversion Recovery Hyperintensities Related to Delayed Gadolinium Leakage After Stroke. Neurology. 2021 Nov 23;97(21):1000-1001. doi: 10.1212/WNL.0000000000012854. Epub 2021 Sep 23.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#相关性#
54
#Neurol#
59
学习
59
#血脑屏障#
60
学习
70