Stroke:缺血性卒中后静脉溶栓与降低痴呆发生率的关系
2022-01-02 MedSci原创 MedSci原创
首次缺血性卒中后溶栓治疗与痴呆发生率降低独立相关。在评估缺血性卒中患者溶栓的风险/益处时,应将事件性痴呆视为相关结局。
静脉溶栓的使用与患者临床结局的改善相关。溶栓是否与卒中后痴呆发生率降低相关尚不明确。

近日,心血管疾病领域权威杂志Stroke上发表了一篇研究文章,研究人员试图使用观察性试验来估计首次缺血性卒中后溶栓是否与痴呆发生率降低相关。

研究人员纳入了安大略省卒中登记处的首例缺血性卒中患者,这些患者既往未被诊断出痴呆症。该研究的主要结局是由经过验证的诊断算法确定的痴呆事件。研究人员采用治疗加权Cox比例风险模型的逆概率来估计卒中后1年和5年溶栓和痴呆事件之间关联的特定原因风险比。
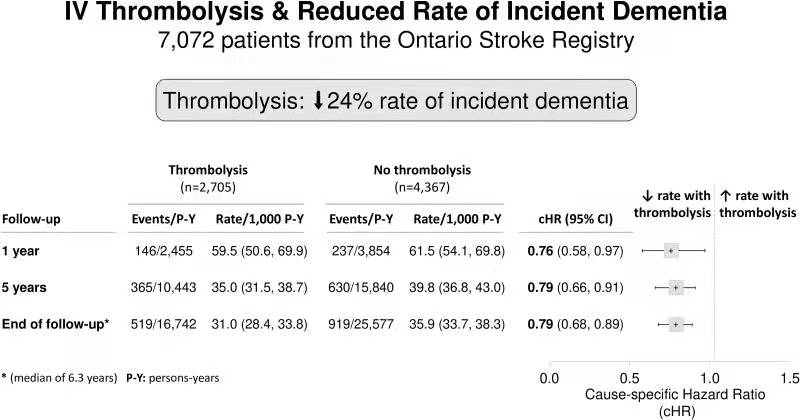
2003年7月至2013年3月期间,研究人员共纳入了7072例缺血性卒中患者,其中女性为3276例(46.3%)患者,平均年龄为71.0(SD为12.8)岁。总体而言,队列中38.2%的患者(n=2705)接受了溶栓治疗,其中77.2%的患者(n=2087)在卒中发作后3小时内进行了溶栓治疗。在卒中后的第一年,溶栓治疗可使痴呆的发生率相对降低24%(病因特异性风险比为0.76[95%CI为0.58-0.97])。这种相关性在5年(特定病因风险比为0.79[95%CI为0.66-0.91])和随访结束时(中位时间为6.3年;特定病因风险比为0.79[95%CI为0.68-0.89])仍然显著。
由此可见,首次缺血性卒中后溶栓治疗与痴呆发生率降低独立相关。在评估缺血性卒中患者溶栓的风险/益处时,应将事件性痴呆视为相关结局。
原始出处:
Joshua O. Cerasuolo.et al.Intravenous Thrombolysis After First-Ever Ischemic Stroke and Reduced Incident Dementia Rate.stroke.2021.https://www.ahajournals.org/doi/10.1161/STROKEAHA.121.034969
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言








#静脉#
47
#缺血性#
59
#缺血性卒#
77
#发生率#
43
#卒中后#
60
受教,非常棒
70
老年性痴呆,未来还是希望借助神经电生理吧,也许更为有效!
48