Circulation:对CREST模型早期预测非STEMI患者心脏骤停后循环病因学死亡风险的推导和验证。
2017-11-23 fengxiangxin MedSci原创
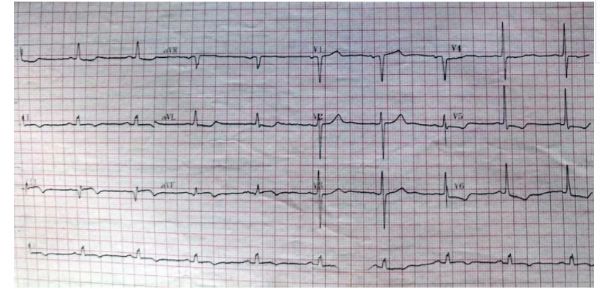
无ST段抬高型心肌梗死(STEMI)患者在进行心肺复苏成功后,尚没有实用工具可以立即量化其循环病因学死亡(CED)的风险。为了快速确定风险并促进将患者分类到个性化治疗途径中,研究者开发并验证了他们的预测模型。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言









#EST#
74
#STEMI患者#
77
学习了谢谢分享!!
120
#死亡风险#
71
#STEM#
59
#CRE#
78