Blood:与来那度胺/泊马度胺获得性耐药相关的多重CRBN变异!
2021-01-18 MedSci原创 MedSci原创
出现对所有可用疗法的耐药性是提高骨髓瘤存活率的主要挑战。Cereblon(CRBN)是多种药物的重要结合蛋白,这些药物包括广泛应用于骨髓瘤的免疫调节药物(IMiD)和新型CRBN E3连接酶调节剂(C
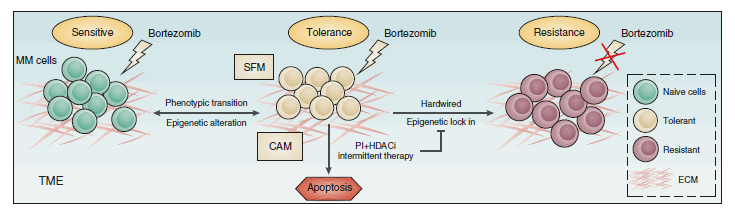
出现对所有可用疗法的耐药性是提高骨髓瘤存活率的主要挑战。Cereblon(CRBN)是多种药物的重要结合蛋白,这些药物包括广泛应用于骨髓瘤的免疫调节药物(IMiD)和新型CRBN E3连接酶调节剂(CELMoD),以及某些正在开发中的用于治疗一系列疾病的针对嵌合体的蛋白水解(PROTAC)类药物。
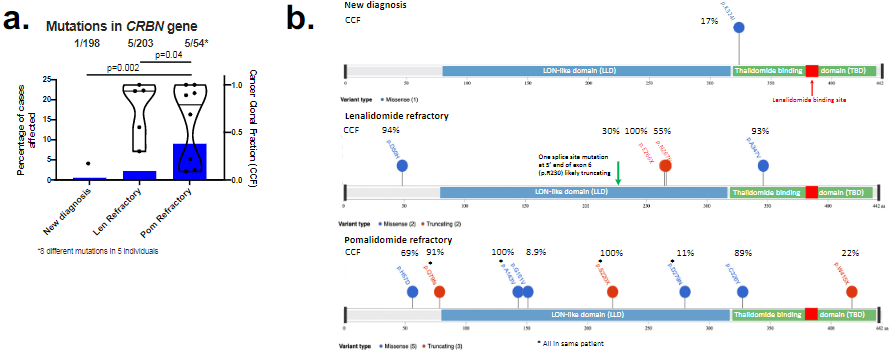
本研究使用来自455名患者的全基因组测序(WGS)数据和来自655名患者的RNA测序(RNAseq)数据,这些患者来自三个不同的队列:一个新确诊队列(WGS,n=198;RNAseq,n=437)、一个来那度胺(LEN)-难治队列(WGS,n=203;RNAseq,n=176)和一个泊马度胺(POM)-难治队列(WGS,n=54;RNAseq,n=42)。
不同患者的CRBN变异
经分析发现,随着IMiD的逐渐暴露,3种CRBN变异(即点突变、拷贝丢失/结构变异和一个特定的变异转录本[10号外显子剪接])的频率逐渐增加,直到几乎三分之一的患者在对POM耐药时都会出现CBRN变异。
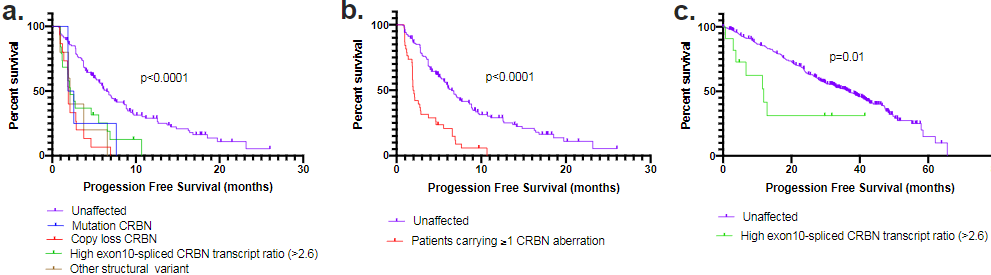
CRBN变异与多发性骨髓瘤患者预后的相关性
研究人员发现,这3种CRBN变异都与那些已经对LEN耐药的患者采用POM治疗时的预后较差有关,包括那些有基因复制丢失和结构变异的患者,这一发现是以前没有描述过的。
综上,本研究是第一个也是最大的一个全面分析骨髓瘤患者在治疗过程中CBRN变异的数据集。本研究结果将有助于指导患者选用CRBN靶向药物进行序贯治疗。
原始出处:
Gooding Sarah,Ansari-Pour Naser,Towfic Fadi et al. Multiple cereblon genetic changes are associated with acquired resistance to lenalidomide or pomalidomide in multiple myeloma. Blood, 2021, 137: 232-237.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#获得性#
76
#获得性耐药#
97
#Crbn#
78
#变异#
65
666
244