JACC:急性主动脉夹层报告--诊断以及入院治疗结果的17年趋势
2015-07-21 崔倩 译 MedSci原创
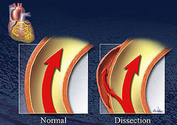
目前急性主动脉夹层(AAD)的诊断、治疗及治疗成果正在发生着变化。本研究对来自于国际急性主动脉夹层的注册表(IRAD)的AAD报告的诊断以及入院治疗结果的17年的发展趋势进行了探讨。 数据来自于1995年12月26日和2013年2月6日之间,28个IRAD中心的4428例患者的数据,并进行了分析。根据患者的招募日期被为数量相等的6组,根据AAD类型被分为

本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言









#JACC#
52
#急性主动脉夹层#
45
#ACC#
59
#主动脉#
42
#动脉夹层#
55
#治疗结果#
48