European Radiology:CCTA中的血管周围脂肪衰减指数究竟有何临床价值?
2022-08-15 shaosai MedSci原创
最近,人们开发了一种新型的使用CCTA测量的无创成像生物标志物,即血管周围脂肪衰减指数(pFAI),可以直观地显示冠状动脉炎症,这是动脉粥样硬化的一个重要驱动因素。
越来越多的证据表明,血管周围脂肪组织(PVAT)在心血管疾病中具有重要的生物学意义,PVAT的定量和定性测量对于确定个体的心脏代谢风险状况至关重要。
心外膜脂肪组织(EAT)作为PVAT的一部分,沉积在心脏周围,代谢活跃且产生各种促炎和抗炎因子。EAT可以通过成像技术进行量化,如超声心动图、心脏磁共振和冠状动脉计算机断层扫描(CCTA)。临床研究表明,使用CCTA检测到的高EAT密度或EAT体积增加与炎症和主要不良心脏事件有关。冠状动脉周围脂肪组织(PCAT)是EAT的血管周围层,尽管在解剖学上有密切的关系,在形态和功能上与EAT不同。
最近,人们开发了一种新型的使用CCTA测量的无创成像生物标志物,即血管周围脂肪衰减指数(pFAI),可以直观地显示冠状动脉炎症,这是动脉粥样硬化的一个重要驱动因素。然而,从CCTA方面反映冠状动脉炎症,EAT密度和血管周围FAI是否相似或不同仍是未知数。
近日,发表在European Radiology杂志的一项研究通过使用对比增强CT图像,探讨了已知或疑似冠状动脉疾病(CAD)患者的血管周围FAI和EAT参数(密度和体积)以及整个冠状动脉血管的血管周围FAI分布之间的相关性,为患者的早期风险分层及个性性治疗方案的制定提供了技术支持。

本研究回顾性地纳入了2019年1月1日-2019年6月1日接受冠状动脉计算机断层造影的已知或疑似CAD患者。对四条主要的心外膜冠状动脉和七个冠状节段的血管周围FAI进行了量化,并测量了EAT密度和体积。
本研究共纳入了192名连续患者(55名无冠状动脉斑块[平均年龄46.4±13.2岁,69.1%为男性],137名有冠状动脉斑块[平均年龄57.9±13.0岁,84.7%为男性)。两组的EAT密度都低于血管周围的FAI,但表现出显著的相关性(- 83.33 ± 4.54 vs. - 78.22 ± 6.52 HU, p < 0.001; r = 0.667 in plaque- patients and - 83.11 ± 4.48 vs. - 77.81 ± 5.63 HU, p < 0.001; r = 0.778 in plaque+ patients)。左主冠状动脉的血管周围FAI最高,其次是左回旋动脉。近端段的血管周围FAI明显高于远端段(所有P<0.05)。此外,斑块的存在并没有改变患者或节段的血管周围FAI。
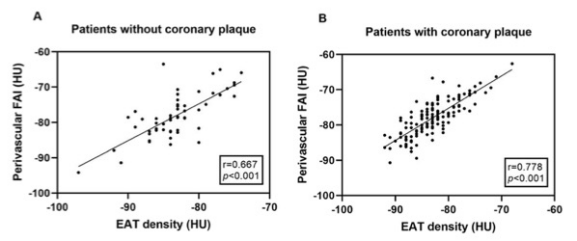
图 无冠状动脉斑块(A)和有冠状动脉斑块(B)的患者,每个病人的血管周围脂肪衰减指数和心外膜脂肪组织密度之间的相关性
本项研究显示,血管周围FAI和EAT密度之间有很好的相关性,而且血管周围FAI显示的数值比EAT密度高。此外,血管周围的FAI在不同的血管和节段之间存在差异。因此,在血管周围FAI研究中考虑血管和节段的混杂因素是必要的。
原文出处:
Wenrui Bao,Chihua Chen,Min Yang,et al.A preliminary coronary computed tomography angiography-based study of perivascular fat attenuation index: relation with epicardial adipose tissue and its distribution over the entire coronary vasculature.DOI:10.1007/s00330-022-08781-9
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#临床价值#
63
#PE#
68
#CTA#
86
#CCT#
67
学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
74