【一般资料】
患者45岁
【主诉】
因半个月来发热、咳嗽、呼吸困难入院。
【现病史】
患者半月前开始觉疲乏无力、低热、未引起注意,后体温逐渐升高,达38~39℃,出现干咳,右侧胸痛,因吸气而加重,伴有盗汗,三天来出现呼吸困难,喘憋、胸闷、活动后加重,而到医院检查,门诊化验血白细胞正常,胸透有胸腔积液,而收入院诊治。
【体格检查】
一般情况尚好,可以平卧,体温38.2℃,血压110/70mmHg,呼吸20次/分,脉搏90次/分,皮肤无黄染、皮疹及出血点,浅表淋巴结不大,心率90次/分,律齐,各瓣膜区未闻杂音,右下肺叩浊,呼吸音减低,未闻干湿啰音及胸膜摩擦音,腹平软,无压痛,肝脾不大,无移动性浊音。
【辅助检查】
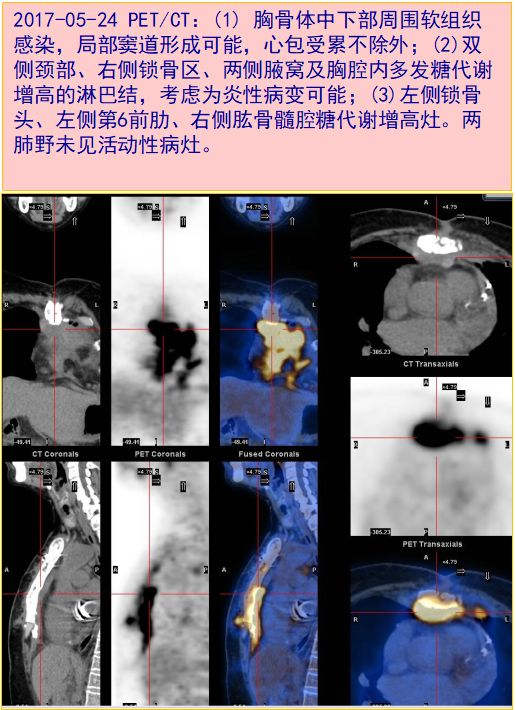
白细胞13×109/L,中性粒细胞占52%,淋巴细胞占48%,血红蛋白120g/L,血小板120×109/L,尿常规正常,血沉78mm/第一小时,肝肾功能正常,胸片显示右侧胸腔中等量积液,左上有钙化灶,心电图正常。胸腔穿刺:胸水外观为淡黄色,微浑,比重1.20,蛋白定性阳性,蛋白定量4.5g/dl,细胞数1500×106/L,分类淋巴细胞占80%。
【治疗】
入院诊为结核性胸膜炎,给以抗结核治疗,体温逐渐下降,胸痛减轻。入院后10天患者出现双下肢无力,发凉,而且逐日加重,以致行走困难,腰背疼痛,当时检查胸椎局部有压痛,局部略有隆起,为除外胸、腰椎疾患而做胸腰椎X线片检查,报告为胸椎结核,寒性脓疡形成,椎体明显破坏,准备骨科手术治疗,尚未转至骨科时,患者出现下肢完全瘫痪,排尿困难,最后诊断为胸椎结核合并截瘫、结核性胸膜炎,转入骨科进行手术治疗。
【讨论】
误诊原因与教训1﹒患者腰背酸痛,已有半年余,下肢无力、发麻已有两个月余,而患者自认为是着凉,劳累引起,未给以注意。医生在询问病史时,也未问到腰背疼痛史,而且体检也未做脊柱四肢检查,当X线片诊断为胸椎结核时,才发现患者胸椎下段有明显压痛和叩击痛。此次住院因发热、咳嗽、胸痛,来医院治疗,病情已拖延数月,使胸椎结核病变到严重破坏程度,引起截瘫,令人痛心,如果在半年前就引起患者注意并得到医生的全面检查,及时作骨X线检查,明确诊断,及时治疗,可能不会出现截瘫的后果。全面的体格检查是医生诊断疾病的基本功,从一般状态、皮肤黏膜、淋巴结、头颈部、胸部、腹部、脊柱四肢,一直到神经系统,不管患者主诉是哪一系统疾病,都应作全面检查,当然根据病情要有重点检查的部位。2﹒医生在诊治病人时,还应仔细询问病史,患者主诉有疲乏无力感,应追问“无力”到什么程度,伴随什么症状,启发病人回忆疾病发生发展的过程,当然,很多疾病都会出现疲乏无力,但该患者无力到迈出1~2步都困难,而且下肢还有麻木的感觉,当时应做神经系统详细的检查。该患者结核性胸膜炎的发生,实质上是由胸椎结核引起的,原发病在胸椎病变上。3﹒不明原因腰背酸痛,伴有低热、无力、体重下降一定要警惕脊椎结核的可能,做细致的体格检查,及时作X线检查。
版权声明:
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言









#胸膜炎#
51
#腰酸#
51
#胸膜#
44
#结核性#
65
好文献.学习了
70
#结核#
45