病例分享:心梗之外的无声杀手 ——从1例跌宕起伏的急性胸痛病例说开去
2018-04-05 首都医科大学附属北京安贞医院 高玉龙 李志忠 魏县中医院 王志强 中国医学论坛报今日循环
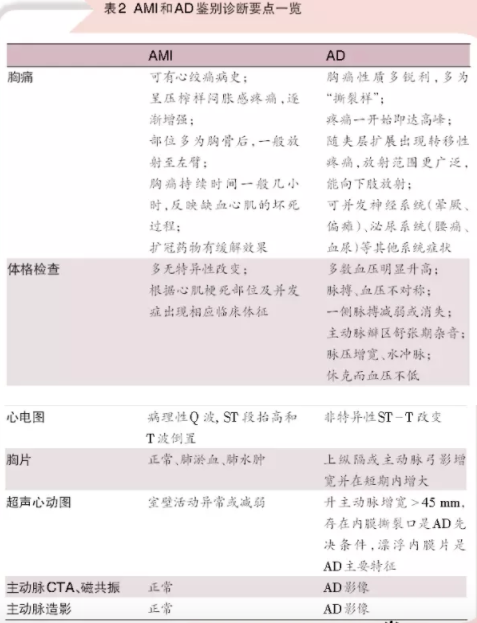
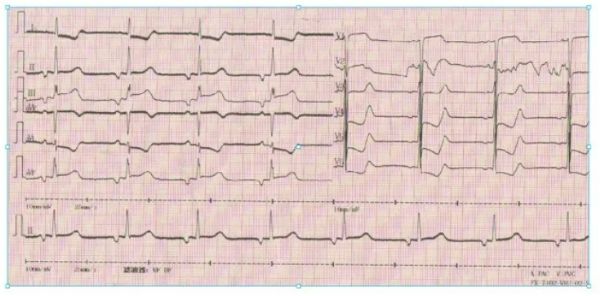
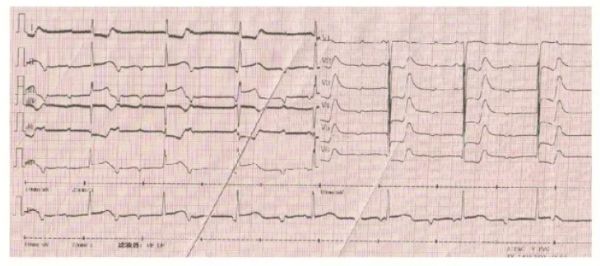
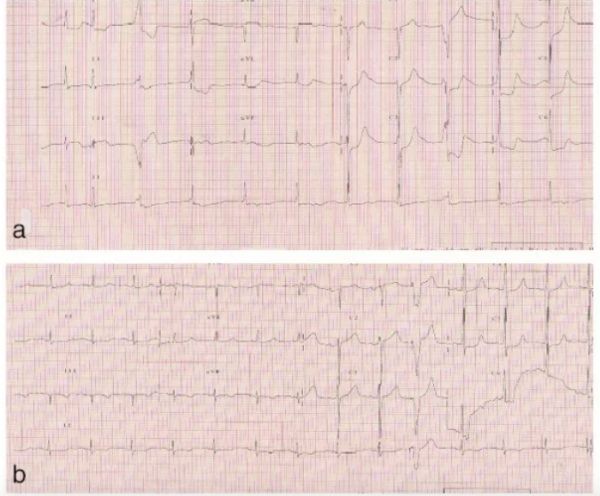
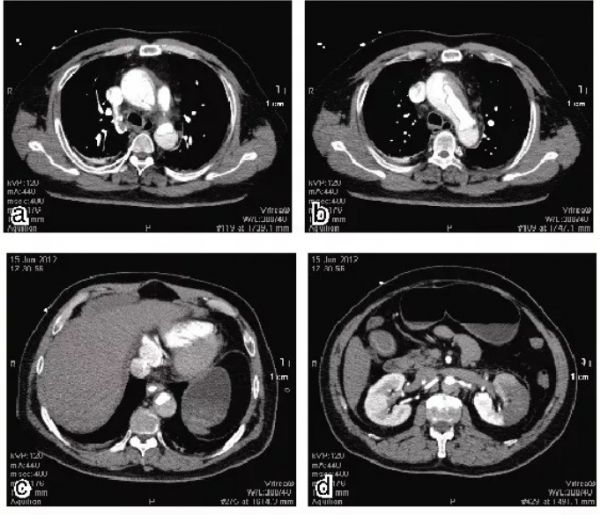
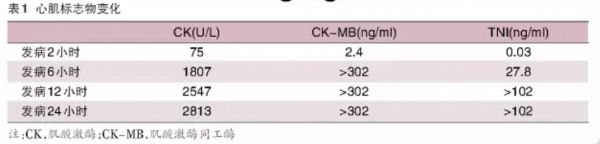
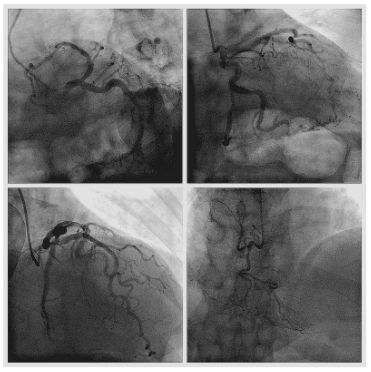
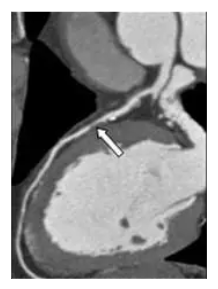
急性胸痛是急诊内科最常见的疾病。调查发现,急性胸痛在门诊接诊的患者中占20%,在救护车接诊的患者中占69%,在急诊室接诊的患者中占45%。对于急性胸痛首先应明确是否由潜在致死性疾病引起,如急性心肌梗死(AMI)、主动脉夹层(AD)、急性肺栓塞和张力性气胸等,需要在短时间内作出恰当诊断和处理。若误诊或漏诊,会导致严重后果。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










好文献.学习了
0
学习了.谢谢分享
93
学习了
90
学习了.获益匪浅.感谢分享
87
学习主动脉夹层和心肌梗塞的鉴别
91
学习了
49