Nature:艾滋病治疗新药3BNC117的疗效值得期待
2016-08-01 佚名 来宝网
虽然在艾滋病的治疗上已经取得了重大进步,可以通过抗逆转录病毒药物对疾病进行控制,但是目前仍没有治愈方法。并且目前的药物也有很多不足:必须每日服用,一生服用,常常导致长期的不良反应。近日科学家研制出了一种抗体用于治疗艾滋病,这种药物有长时间的疗效,可以降低患者的用药频率。该研究成果发表在近日的《Nature》期刊,该抗体的名字目前定为3BNC117,能够有效地延迟由于患者暂时停止服用抗逆转录病毒药物
虽然在艾滋病的治疗上已经取得了重大进步,可以通过抗逆转录病毒药物对疾病进行控制,但是目前仍没有治愈方法。并且目前的药物也有很多不足:必须每日服用,一生服用,常常导致长期的不良反应。
近日科学家研制出了一种抗体用于治疗艾滋病,这种药物有长时间的疗效,可以降低患者的用药频率。
该研究成果发表在近日的《Nature》期刊,该抗体的名字目前定为3BNC117,能够有效地延迟由于患者暂时停止服用抗逆转录病毒药物而引起的疾病进展,抗逆转录病毒治疗时目前HIV的标准治疗方法。
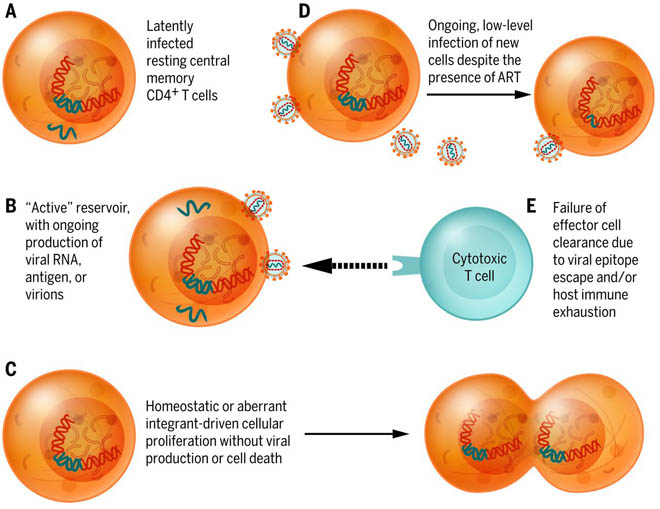
该抗体分离自一位HIV感染的患者,具体来自该患者的可以有效抗击HIV的某个细胞克隆。HIV主要感染人的CD4 T细胞,这些细胞是免疫系统保护人免受感染的细胞。该抗体可以阻止HIV对CD4 T细胞的感染。
抗逆转录病毒药物的作用机理是抑制病毒复制,但是病毒仍然会占领人体,大部分的HIV都集中在CD4细胞中。如果患者停止服用抗逆转录病毒药物,HIV就会从这些细胞中释放出来,造成疾病的反弹。
这一次,研究者在13例HIV感染的患者中进行了临床试验,这些患者均接受了抗逆转录病毒药物治疗,并且成功控制住了病情。该研究的目的是考察在患者停止服用抗逆转录病毒药物后,疾病反弹的时间。研究结果显示,该抗体可以将疾病反弹的时间推迟到大约10个星期,而对照组只能推迟3个星期。
接下来,研究者将探讨该抗体和其他HIV治疗方案联合应用时的效果。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#Nat#
45
学习了,赞一个!
67
学习了,赞一个!
56
学习了,赞一个!
77
学习了,赞一个!
69
值得研究
71