Cell Death & Disease:CCL5能够促进前列腺癌干细胞和转移
2020-04-27 AlexYang MedSci原创
前列腺癌干细胞(PCSCs)在前列腺进展和转移中具有重要作用,是前列腺癌治疗的一个障碍。肿瘤相关的巨噬细胞(TAMs)是肿瘤微环境(TME)中最丰富的免疫细胞群。PCSCs与TAMs之间互作和信号网络
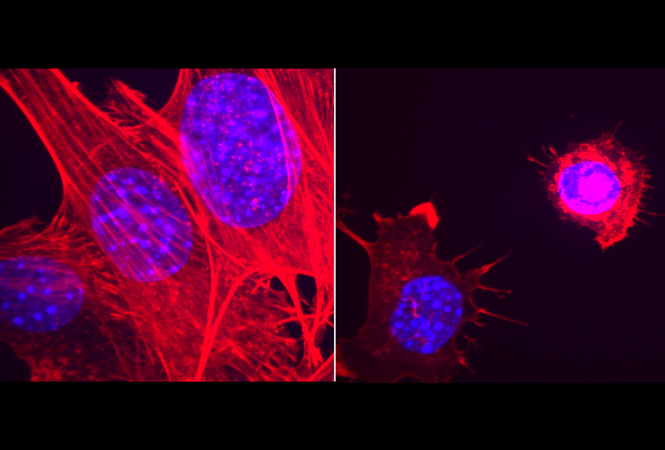
前列腺癌干细胞(PCSCs)在前列腺进展和转移中具有重要作用,是前列腺癌治疗的一个障碍。肿瘤相关的巨噬细胞(TAMs)是肿瘤微环境(TME)中最丰富的免疫细胞群。PCSCs与TAMs之间互作和信号网络的系统调查能够帮助寻找能够抑制PCSCs和转移的关键靶标。
最近,有研究人员阐释了TAMs分泌的CCL5能够显著的促进前列腺癌细胞的迁移、浸润和上皮-间质转化(EMT),以及PCSC在体外的自我更新。QPCR筛选验证了STAT3是CCL5处理前列腺癌细胞后响应最显著的基因。RNA测序和机制探索进一步阐释了CCL5能够通过激活β-连环蛋白/STAT3信号促进PCSCs的自我更新和前列腺癌转移。明显的是,在TAMs中CCL5的敲除不仅能够显著的抑制前列腺癌异种种植的生长和骨转移,同时也抑制了体内试验中PCSCs的自我更新和致瘤性。最后,临床调查和和生物信息学分析表明了前列腺癌患者中,CCL5的高表达与高格林森等级、不良预后、转移以及PCSCs活性的增加有关。
最后,研究人员指出,TAMs/CCL5能够通过激活β-连环蛋白/STAT3信号促进PCSCs的自我更新和前列腺癌转移。他们的研究为开发TAMs/CCL5作为PCSCs清除和转移性前列腺癌预防的潜在分子靶标提供了新的理论基础。
原始出处:
Renlun Huang, Shengqi Wang, Neng Wang et al. CCL5 derived from tumor-associated macrophages promotes prostate cancer stem cells and metastasis via activating β-catenin/STAT3 signaling. Cell Death & Disease. 16 April 2020
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












已拜读,受益匪浅。
80
#CEL#
63
#Cell#
66
#Dis#
58
干细胞是热点,但是进入临床仍然需要时间和临床疗效验证哦
69
#Death#
50
#癌干细胞#
0
#CCL5#
71
前列腺癌相关研究,学习了,谢谢williamhill asia
86