Cancer Cell:治疗新潜力药物—让癌细胞“得瑟”而死
2015-08-12 佚名 生物谷
图:左为对照组癌细胞,右为经MCB-613处理的癌细胞癌细胞的分裂繁殖速度已经超乎正常,那如果给点刺激,让癌症细胞长得再快点会出现什么情况?——答案是会“得瑟”而死。这种过度刺激肿瘤生长关键蛋白的候选药物或将作为一种新的方法治疗多种癌症。该方法的工作原理是让癌细胞在应激边缘“不堪重负”而死。这篇文章发表在最新的Cancer Cell杂志。本文资深作者,David Lonard是美国贝勒医学院细胞
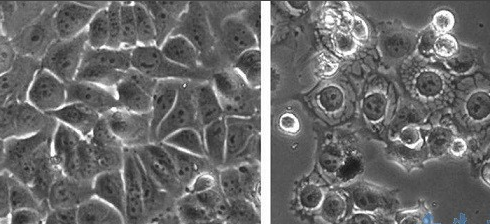
图:左为对照组癌细胞,右为经MCB-613处理的癌细胞
癌细胞的分裂繁殖速度已经超乎正常,那如果给点刺激,让癌症细胞长得再快点会出现什么情况?——答案是会“得瑟”而死。这种过度刺激肿瘤生长关键蛋白的候选药物或将作为一种新的方法治疗多种癌症。该方法的工作原理是让癌细胞在应激边缘“不堪重负”而死。这篇文章发表在最新的Cancer Cell杂志。
本文资深作者,David Lonard是美国贝勒医学院细胞和分子生物学教授,他表示说:“目前还没有任何被提议或者开发的药物是通过刺激癌基因来达到治疗目的。williamhill asia 的原型药物能在多种类型的癌症中发挥作用,这将可能作为癌症药物库中新的而更普遍的选择。”
肿瘤细胞需要获得癌基因突变,以支持它们的生长和生存。大量的研究都集中在识别致癌基因,作为癌症药物靶标。致癌基因中,类固醇受体共激活因子(SRC)家族成员尤其具有作为治疗靶标的希望,因为这些蛋白质坐落在使癌细胞快速增长、扩散、并获得耐药性的关键信号传导途径中。在之前的研究中,Lonard和另一位同事Bert O'Malley通过筛选大量的化合物,在动物模型中确定了一种SRC抑制分子,能杀死多种癌细胞,抑制肿瘤生长。这些化合物是类似于常规的抑制癌基因的药物。但是,他们有一个违反直觉的想法:如果他们能破坏关键信号通路,过度刺激SRC,会不会杀死癌细胞?毕竟癌细胞在很大程度上依赖SRC精细调节各种细胞活动,所以SRC刺激可能与SRC抑制在扰乱癌细胞信号活性的平衡一样有效。
为了验证这个想法,他们筛选成千上万的化合物,以确定一个有效的SRC激活物——被称为MCB-613。MCB-613能杀死人乳腺癌、前列腺癌、肺癌和肝癌细胞,同时保留正常细胞。当研究人员向13只乳腺癌小鼠注射MCB-613后,这个化合物几乎完全消除了肿瘤的生长,同时没有引起毒性,而对照组的14只小鼠肿瘤在7周内长到了原来的3倍以上大小。

那具体的工作机制是什么?MCB-613使内质网上的未折叠蛋白质大量堆积。因为要支持细胞迅速繁殖,癌细胞必须合成大量的蛋白质,使负责折叠蛋白的内质网承受沉重的工作量。当过度刺激SRC后,给已经达到最大工作量的ER再添额外负担,造成了大量未折叠蛋白的积累,触发细胞的应激反应,导致毒性分子活性氧的增多。
总得来说,再提升已经在癌细胞能十分活跃的SRC活性,使得已经在最大压力承受下的细胞应激反应系统更加苦不堪言,出现选择地细胞死亡。在未来的研究中,研究人员将继续深入探索SRC杀死癌细胞的机制,并筛选更好的SRC激活剂。
原文出处:
Yang Yu, Dar-Chone Chow,et al.Characterization of a Steroid Receptor Coactivator Small Molecule Stimulator that Overstimulates Cancer Cells and Leads to Cell Stress and Death.Cancer Cell.2015
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#cancer cell#
44
#CEL#
35
#Cell#
40
太新颖了吧
156
会对机体产生怎么影响?
99
这个想法超前
124
#癌细胞#
37