CRP、血脂四项只用来看感染和高脂血症?组合使用竟可预示癌症患者结局!
2022-07-01 MedSci原创 MedSci原创
BMC Cancer:癌症患者全身炎症和胰岛素抵抗的预后重要性:前瞻性多中心研究.
炎症和胰岛素抵抗(IR)在包括癌症在内的各种慢性疾病中起重要作用。癌症仍然是全世界死亡的主要原因。根据《2020年全球癌症统计数据》,2020年估计有1930万例新癌症诊断和1000万例癌症相关死亡。在许多研究中,全身性炎症的标志物与癌症风险和死亡率增加有关,包括食道癌、胃癌、结直肠癌、肝癌、胰腺癌、膀胱癌和肺癌。流行病学研究表明,C反应蛋白(CRP)循环水平升高不仅预示着癌症的流行,而且与明显健康的人群未来患癌症的风险增加有关。

IR被认为是对妊娠、禁食、运动和急性应激环境的生理适应性反应,也存在于各种慢性疾病中,例如肥胖、2型糖尿病(T2D)和癌症恶病质。既往研究表明,许多新颖、间接、廉价且易于获得的替代标志物可以充分预测IR,包括低密度脂蛋白胆固醇与高密度脂蛋白胆固醇(LDL-c/HDL-c,LHR)比值、总胆固醇与高密度脂蛋白胆固醇(TC/HDL-c)比值、甘油三酯与高密度脂蛋白胆固醇(TG/HDL-c)比值和空腹甘油三酯葡萄糖(TyG)指数。在这些指标中,癌症患者的最佳IR预后指标尚不清楚。
全身性炎症和胰岛素抵抗(IR)通常与癌症预后不良有关。本研究旨在探讨替代性全身炎症和IR指数在癌症患者中的预后价值。
这项多中心前瞻性研究包括5221名癌症患者,平均年龄为59.41±11.15岁,其中3061人(58.6%)为男性。替代IR指数包括低密度脂蛋白胆固醇与高密度脂蛋白胆固醇(LHR)的比值,总胆固醇与高密度脂蛋白胆固醇(TC / HDL-c)的比率,甘油三酯与高密度脂蛋白胆固醇(TG / HDL-c)的比率以及空腹甘油三酯葡萄糖(TyG)。

在这项研究中,患者的中位生存时间为44.5(40.5-51.4)个月,12个月期间的总死亡为1115(53.7%),每1000名患者随访的患者年中有196个死亡事件。ROC预后曲线和C指数表明,LHR的预后值优于其他IR指数。

高C反应蛋白(CRP)(HR,1.51;95% CI:1.38-1.65)和高LHR(HR,1.20;95%CI:1.06-1.37)患者的多变量调整风险比(HR)在总生存期(OS)中较高。高CRP和LHR患者的死亡率比低CRP和LHR患者的死亡率高1.75倍。
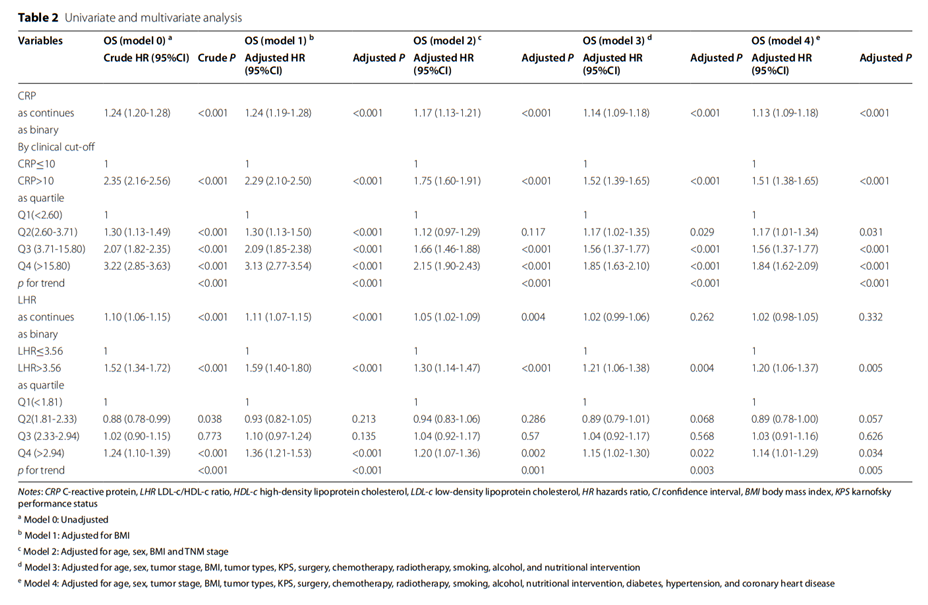
总的来说,这项研究强调了全身炎症和IR在癌症患者预后中的重要性。LHR在癌症患者中的预后值优于TG / HDL-c,TC / HDL-c和TyG。此外,本研究结果表明,CRP和LHR可以预测癌症患者的生存。高CRP和高LHR都预测了较差的OS。高CRP和LHR患者的死亡率比低CRP和低LHR患者的死亡率高1.75倍。
原文来源:
Ruan GT, Xie HL, Gong YZ, Ge YZ, Zhang Q, Wang ZW, Zhang X, Zhang HY, Tang M, Song MM, Zhang XW, Yang M, Chen YB, Yu KY, Deng L, Wang KH, Cong MH, Shi HP. Prognostic importance of systemic inflammation and insulin resistance in patients with cancer: a prospective multicenter study. BMC Cancer. 2022 Jun 25;22(1):700. doi: 10.1186/s12885-022-09752-5. PMID: 35752767; PMCID: PMC9233357.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言














最后一段文字没有显示出来
127
#CRP#
88
#癌症患者#
96
#患者结局#
89
#高脂#
121
放之四海而皆准!
111