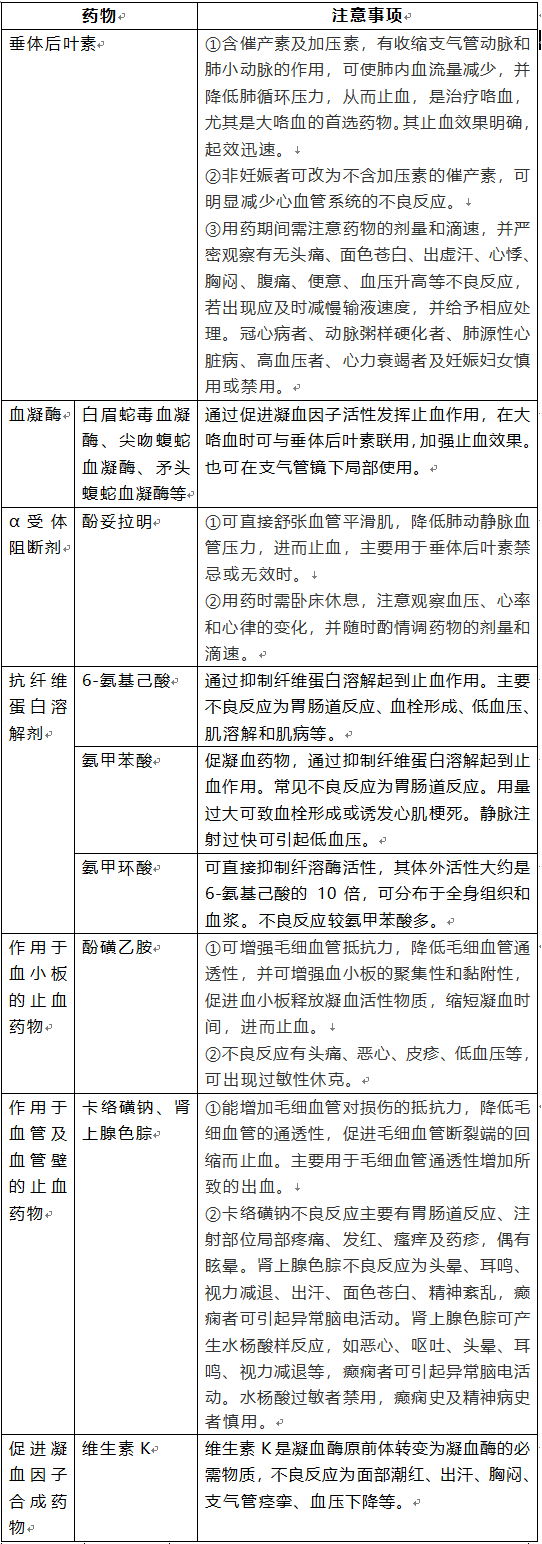
咯血的治疗药物选用及注意事项
2020-01-19 高丽丽 医学之声
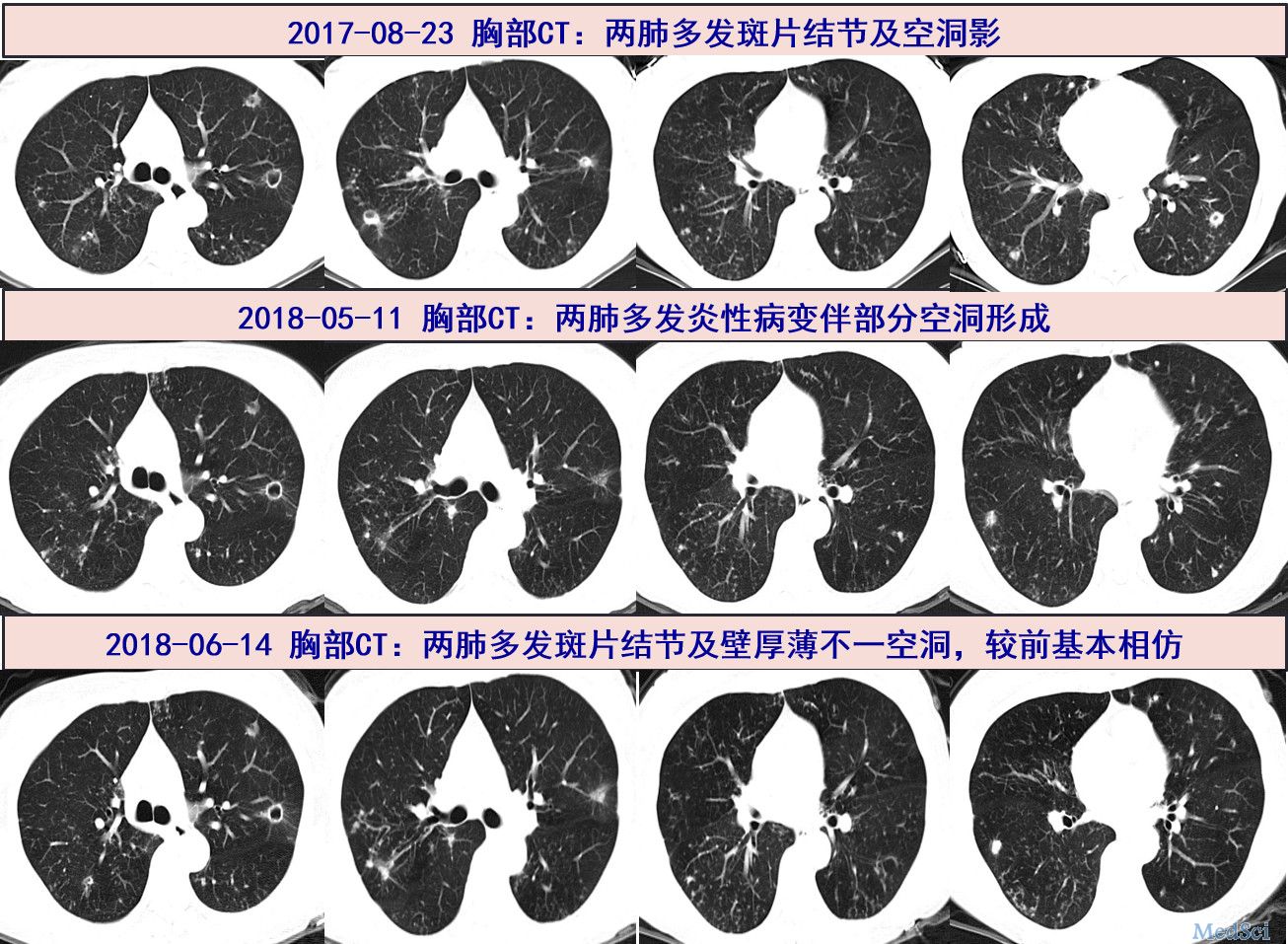
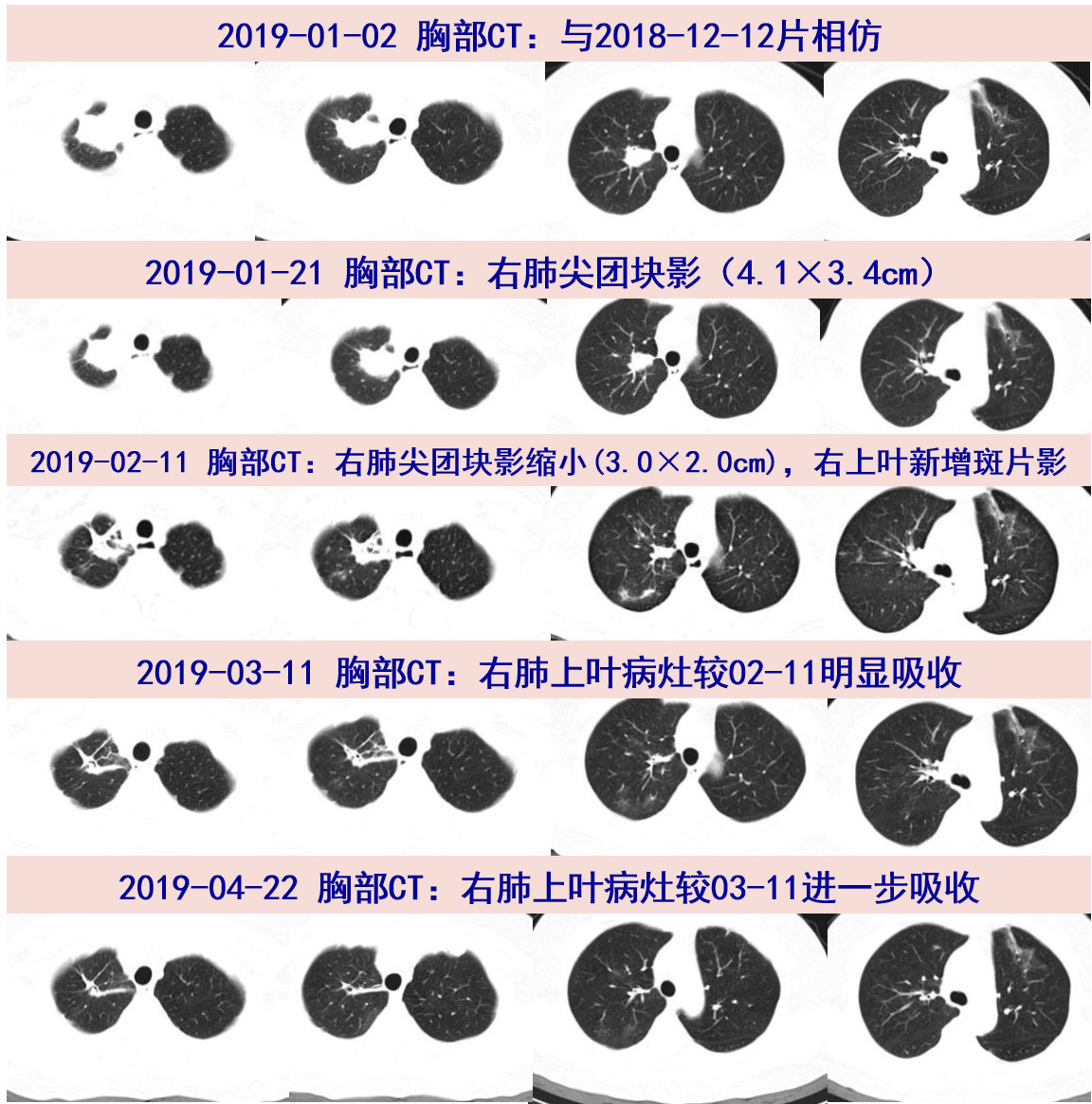
咯血是喉及喉以下呼吸道任何部位的出血,经口腔排出的一种临床症状,通常规定24h内咯血大于500mL(或1次咯血量100mL以上)为大量咯血,100-500mL为中等量咯血,小于100mL为小量咯血。其中支气管扩张、结核、肺曲霉菌病、坏死性肺炎、隐源性咯血和肺癌被认为是大咯血最常见的原因。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










学习
7
#注意事项#
60
#治疗药物#
46
#咯血#
61