Nat Rev Drug Discov:AAV基因治疗神经系统疾病的进展与挑战
2018-08-17 陈婉仪 医麦客
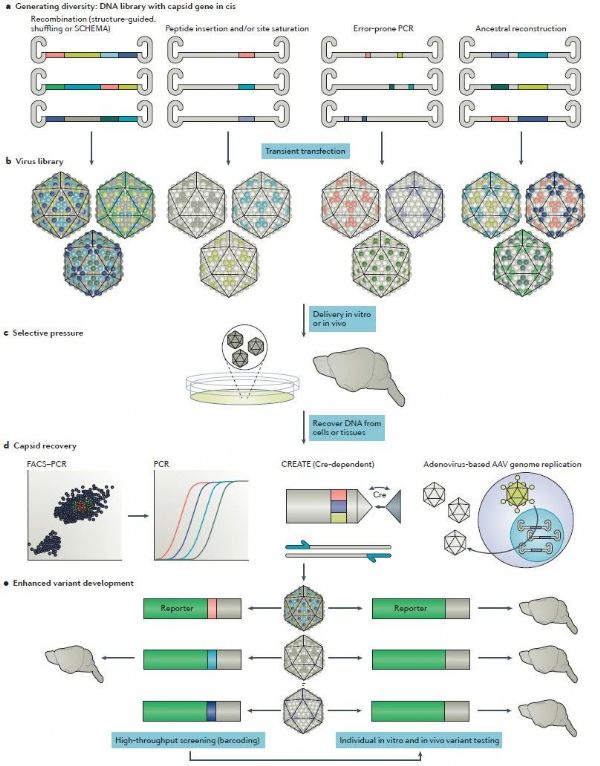
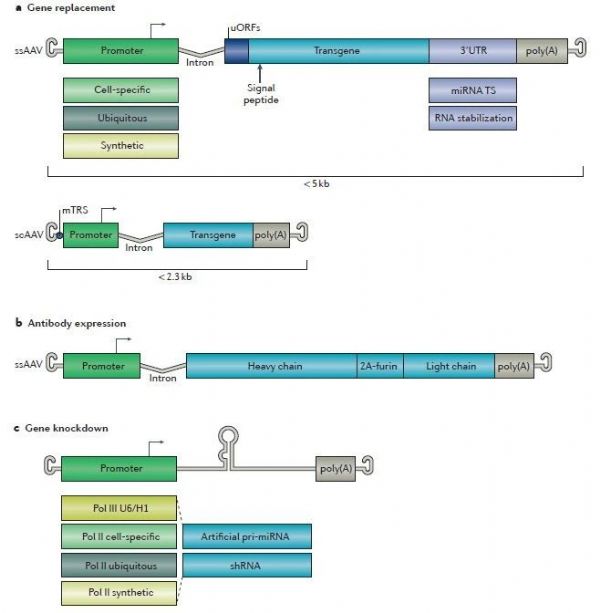
8月10日,Nature Reviews上发表了一篇关于AAV基因治疗神经系统疾病的进展与展望,通讯作者是Voyager Therapeutics的首席科学官Dinah WY Sah。文中探讨了未来设计和开发治疗性AAV载体的关键考虑因素和挑战,并且列举了最近的临床进展。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#Drug#
52
#Dis#
56
学习了谢谢
98
哈哈哈,学习了
86
#Nat#
55
#AAV#
52
#神经系统#
39
#ISC#
54
AAV基因治疗神经系统疾病。
90
学习了,谢谢分享
76