JCEM:家族性高胆固醇血症突变的表型预测比较分析!
2018-02-04 xing.T MedSci原创
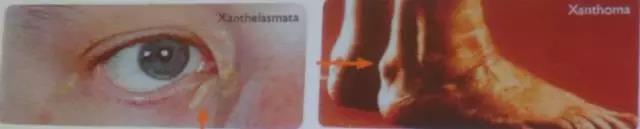
由此可见,DLCN、SB和MEDPED标准是转诊至脂质门诊患者中FH突变的有效预测指标,但这些表型标准之间的一致性仅为中等。单独使用治疗前LDL-胆固醇和肌腱黄瘤可能对决定谁应该进行FH基因检测是特别有用的。
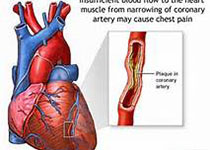
诊断家族性高胆固醇血症(FH)的金标准是鉴定致病性基因突变。然而,基因检测是昂贵的,并不是广泛可用。近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,研究人员旨在比较荷兰血脂诊所网络(DLCN)、西蒙布鲁姆(SB)、早期诊断预防早期死亡(MEDPED)和美国心脏协会(AHA)标准在预测FH发生基因突变方面的有效性。
该研究由转诊至脂质诊所进行基因检测的成年人队列组成,主要观察指标包括比值比(OR)、曲线下面积(AUC)、敏感性和特异性。
在885名接受检测的患者中有30%的个体检测到致病的FH-突变。LDL胆固醇水平升高以及肌腱黄瘤个人史或家族史是突变的独立预测因子(ORs范围为5.32-15.2,P<0.001)。预测DLCN和SB定义和MEDPED标准确定的突变(ORs分别为9.4、11.7和10.5)高于AHA标准(OR为4.67)。 DLCN定义(Youden指数为0.487)、MEDPED(0.457)、SB定义(0.274)和AHA标准(0.253)的敏感性和特异性平衡依次显著降低,DLCN定义和MEDPED的AUC明显高于其他标准(P<0.05)。治疗前的LDL-胆固醇和肌腱黄瘤在预测突变上具有最高的AUC。
由此可见,DLCN、SB和MEDPED标准是转诊至脂质门诊患者中FH突变的有效预测指标,但这些表型标准之间的一致性仅为中等。单独使用治疗前LDL-胆固醇和肌腱黄瘤可能对决定谁应该进行FH基因检测是特别有用的。
原始出处:
Dick C Chan,et al. A comparative analysis of phenotypic predictors of mutations in familial hypercholesterolemia.J Clin Endocrinol Metab. 2018. https://doi.org/10.1210/jc.2017-02622
本文系williamhill asia
医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言









#比较分析#
42
#JCEM#
47
#JCE#
38
不错
54
非常好的文章.学习了
66
#高胆固醇血症#
48
#表型#
26
#家族性#
38