Sci Rep:炎性体感应子的表达分析和NLRP12炎性体在前列腺癌中的意义
2017-07-01 AlexYang MedSci原创
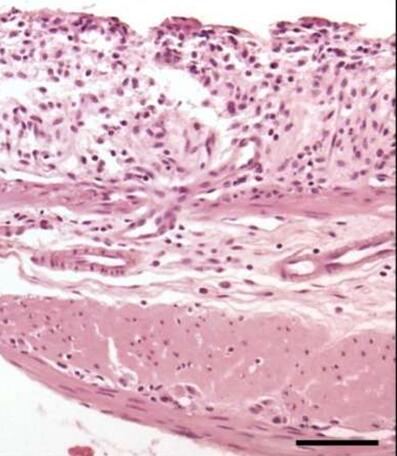
炎性体是多蛋白的复合物,并且可以调节炎症相关的信号通路。尽管炎症在癌细胞的生长过程中扮演着重要角色,在前列腺癌中,炎性体的角色仍旧没有鉴定。最近,有研究人员利用基因表达综合数据库(GEO)公共资料,筛选和分析了炎症体感应子NLRP3、NLRC4、NLRP6、NRLP12和AIM2在前列腺癌组织中的表达情况,并且鉴定了在一组前列腺细胞系中,它们的mRNA表达情况。研究人员对选择的NLRP3和NLRP
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言











#表达分析#
53
#NLR#
48
学习了受益匪浅。
58
学习了受益匪浅
67
学习了受益匪浅
74
研究人员指出,这些数据表明,NLRP12表达的增加与前列腺癌相关,并且支持了NLRP12炎性体复合物可调节炎症细胞因子,促进了炎症在前列腺癌中角色的理解。
64