Int J Nanomed:氯化锂可加速植入物周围成骨
2020-05-08 MedSci原创 MedSci原创
磨损性颗粒引起的炎症性骨溶解以及随之而来的无菌性松动是造成植入物失败和翻修手术的主要原因。多项研究表明,巨噬细胞的极化状态和免疫反应在植入物周围骨溶解和组织修复中起关键作用,但是并无研究探究氯化锂(L
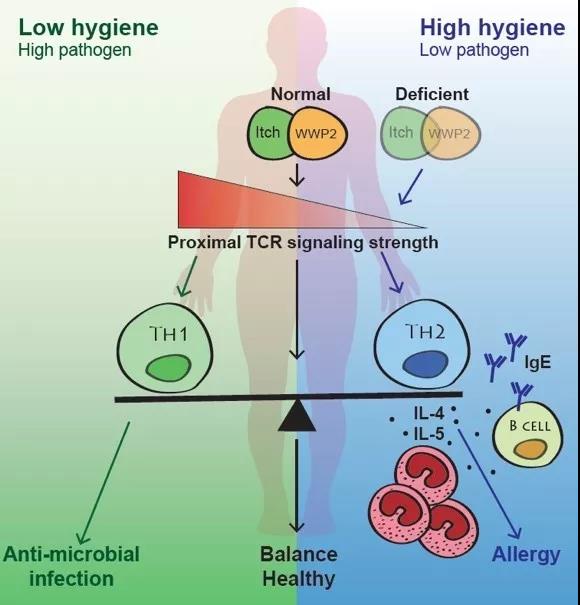
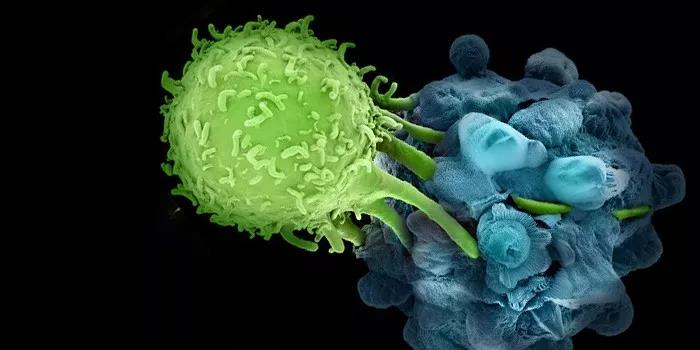
磨损性颗粒引起的炎症性骨溶解以及随之而来的无菌性松动是造成植入物失败和翻修手术的主要原因。多项研究表明,巨噬细胞的极化状态和免疫反应在植入物周围骨溶解和组织修复中起关键作用,但是并无研究探究氯化锂(LiCl)的免疫调节作用,该作用通过抑制破骨细胞和减弱炎症反应而对磨损颗粒引起的溶骨具有保护作用。
在这项工作中,研究人员探究了LiCl对钛(Ti)纳米颗粒刺激的巨噬细胞表型转化的免疫调节能力及其对成骨分化的影响。williamhill asia 首先推测LiCl通过驱动巨噬细胞极化并产生免疫微环境来改善成骨作用,从而减弱了Ti纳米粒子刺激的炎症反应。此外,应用金属纳米颗粒刺激的鼠气袋炎性模型来证实这种体内保护作用。
结果表明,金属纳米颗粒可在体内外明显激活M1表型(促炎性巨噬细胞)的表达并增加促炎细胞因子的分泌,而LiCl将巨噬细胞驱动到M2表型(抗炎性巨噬细胞)并增加抗炎剂的释放和骨相关的细胞因子的表达。这提高了大鼠骨髓间充质干细胞(rBMSCs)的成骨分化能力。此外,williamhill asia 还提供了LiCl抑制磨损颗粒处理的巨噬细胞中p38丝裂原活化蛋白激酶(p38)和细胞外信号调节激酶(ERK)途径的磷酸化的证据。
综上所述,该研究结果表明,LiCl具有免疫调节作用,可通过驱动巨噬细胞极化来减轻Ti纳米颗粒介导的炎症反应并增强rBMSC的成骨分化。因此,LiCl可能是预防和治疗磨损颗粒引起的炎性骨溶解的有效治疗选择。
原始出处:
Chao Yang, Wei Wang, et al., Lithium Chloride With Immunomodulatory Function for Regulating Titanium Nanoparticle-Stimulated Inflammatory Response and Accelerating Osteogenesis Through Suppression of MAPK Signaling Pathway. Int J Nanomedicine. 2019 Sep 12;14:7475-7488. doi: 10.2147/IJN.S210834.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#氯化锂#
58
#锂#
68
#成骨#
77
#植入物#
76
#植入#
67
#Med#
58