Clin cancer res:抗肿瘤坏死因子受体抗体MK-4166治疗晚期实体肿瘤的首次临床试验结果
2021-01-01 MedSci原创 MedSci原创
靶向细胞毒性T淋巴细胞抗原4(CTLA-4)或程序性死亡受体1/程序性死亡配体1的免疫检查点抑制剂(ICI)改善了多种癌症患者的预后,但仍有很大一部分患者对ICI治疗无反应。
靶向细胞毒性T淋巴细胞抗原4(CTLA-4)或程序性死亡受体1/程序性死亡配体1的免疫检查点抑制剂(ICI)改善了多种癌症患者的预后,但仍有很大一部分患者对ICI治疗无反应。
在这项首次在人类中开展的1期试验(NCT02132754)中,研究人员探讨了靶向GITR的人源化IgG1激动剂单克隆抗体MK-4166联合或不联合派姆单抗在晚期实体瘤中的应用。
该研究分为两个队列,剂量/证明队列或扩展队列;剂量递增队列招募转移性实体瘤患者,仅予以MK-4166(0.0015-900mg)或联合派姆单抗(200mg);扩展队列招募晚期黑色素瘤患者。主要目的是明确MK-4166的最大耐受剂量,评估其安全性和耐受性。探索终点包括客观缓解率(ORR)和T细胞T细胞炎症基因表达谱(GEP)分析。
共招募了113位患者(单药治疗48例,联合治疗65例;扩展队列20例)。46位患者(40.7%)出现≥3级不良事件,其中9例(8.0%)与治疗有关。没有观察到与治疗相关的死亡。单药组中有一例剂量限制性毒性事件(膀胱穿孔)被认为与研究药物有关。
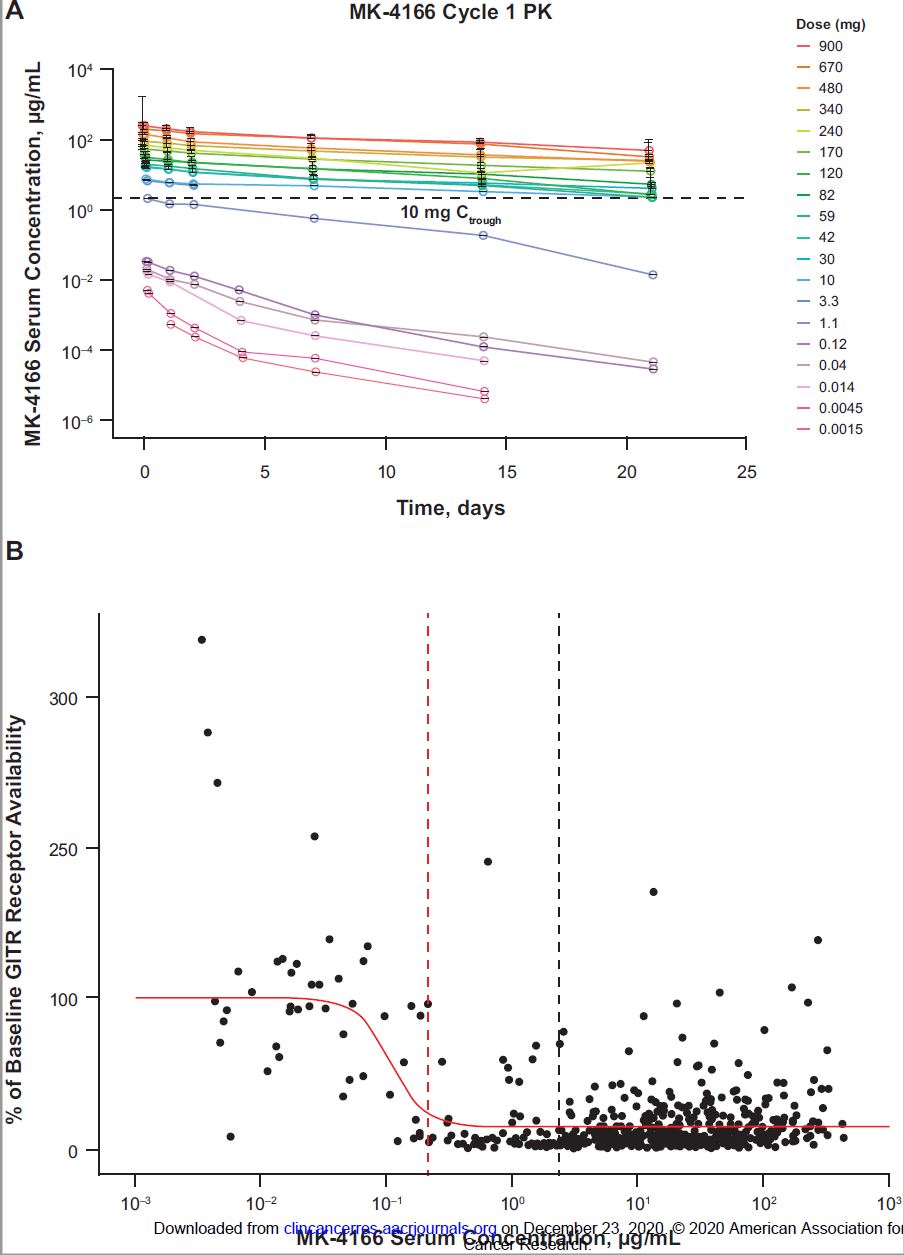
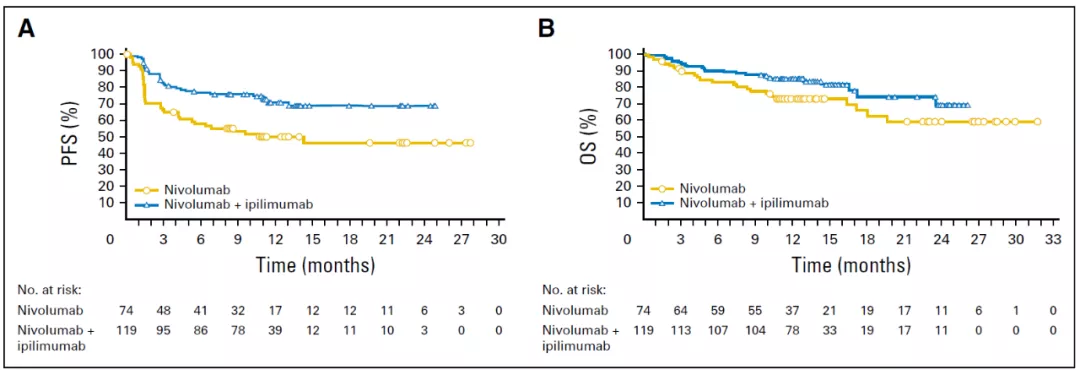
A: MK-4166的血清浓度变化;B:GITR的生物利用度变化
没有达到最大耐受量。MK-4166的药效学显示,随着剂量的增加,GITR在循环T细胞上的利用度降低。
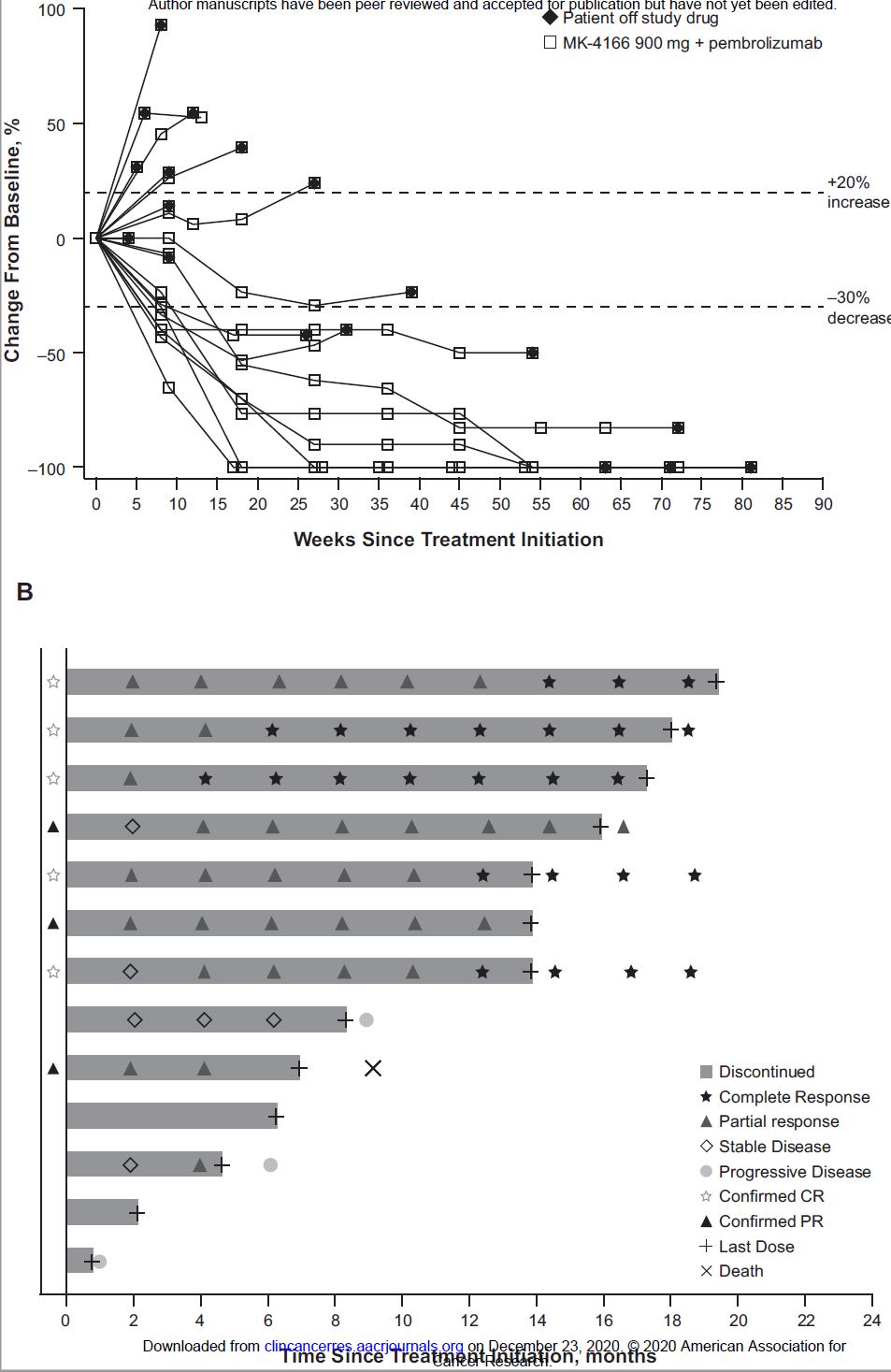
A:扩展队列患者的肿瘤大小变化;B:ICI初治患者的反应及持续时间
在剂量递增队列(n=45)中,联合治疗组有一会患者获得客观缓解(ORR 2.2%)。在扩展队列中,13位ICI初治的黑色素瘤患者中有8位获得缓解(ORR 62%;95% CI 32%~86%;5例完全缓解和3例部分缓解)。7位经ICI预处理的患者均无应答。无论GEP状态如何,ICI初治患者均有较高的应答率。
综上所述,晚期实体瘤患者,单用MK-4166(900mg)或联合派姆单抗治疗的耐受性均在可接受范围内。从联合治疗中获益的主要是ICI初治的黑色素瘤患者。
原始出处:
Papadopoulos Kyriakos P,Autio Karen A,Golan Talia et al. Phase I Study of MK-4166, an Anti-Human Glucocorticoid-Induced Tumor Necrosis Factor Receptor Antibody, Alone or With Pembrolizumab in Advanced Solid Tumors.[J] .Clin Cancer Res, 2020, undefined: undefined.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#晚期实体肿瘤#
58
#坏死#
58
#实体肿瘤#
60
#肿瘤坏死因子#
67
#抗肿瘤坏死因子#
50
#抗肿瘤坏死因子#
69
了解
112
好文章!
120