J Arthroplasty:全关节置换早期乘飞机不增加DVT发生率
2014-07-04 紫川秀第二 丁香园
随着老年人口的增加,行关节置换的患者比例在急剧增多。已经有较多文献报道,关节置换术后患者较容易发生静脉血栓事件。而乘飞机需要较长时间的坐位制动,被认为有较高的血栓发生风险。 如果是全关节置换患者早期需要乘坐飞机进行长距离的转运,是否会增加患者出现血栓的风险呢,美国的纽约的学者就此有趣的问题进行了相关回顾性研究,结果发现,关节置换术后早期乘坐飞机并不会增加患者发生深静脉血栓事件的相关风险,相关
随着老年人口的增加,行关节置换的患者比例在急剧增多。已经有较多文献报道,关节置换术后患者较容易发生静脉血栓事件。而乘飞机需要较长时间的坐位制动,被认为有较高的血栓发生风险。
如果是全关节置换患者早期需要乘坐飞机进行长距离的转运,是否会增加患者出现血栓的风险呢,美国的纽约的学者就此有趣的问题进行了相关回顾性研究,结果发现,关节置换术后早期乘坐飞机并不会增加患者发生深静脉血栓事件的相关风险,相关文章发表在the journal of arthroscopy上。
研究共纳入1465例全关节置换术的患者,随访超过18月。术后对患者进行常规的DVT预防,包括早期活动,机械和药物预防。96%的患者术后接受阿司匹林作为单独的药物预防措施,而其余患者接受抗凝药物预防(表1)。
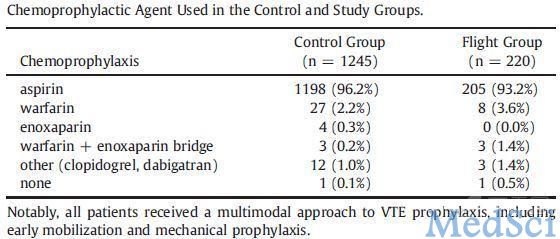
上述患者中,共220例患者(15%)在全关节置换术后2.9天乘坐飞机(图1),而其余1245例患者未乘坐飞机,比较两组患者的人口统计学数据,并进行组间DVT发生率的比较。

结果发现,乘飞机组患者出现症状性DVT,PE,VTE的数量分别为2例(0.9%),1例(0.5%)和3例(1.4%);而未乘飞机患者出现症状性DVT,PE,VTE的数量分别为5例(0.4%),10例(0.8%),15例(1.2%)。组间比较两组数据,无显著性差异。
研究者在讨论中分析,本研究是第一个报道飞行是否会增加关节置换术后静脉血栓发生率的文献报道,本研究证据强度较高的方面包括:入院研究的样本量较大;所有病例均来源一个治疗组;治疗入选患者未经特别筛选,保证了数据的全面性。
鉴于目前临床上并没有此类情况的指导性文件,作者推荐,参照本研究的结论,全关节置换术后的患者在进行规范化的抗凝治疗后可允许早期乘坐飞机进行短距离的飞行。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言








#置换#
49
#发生率#
48
#DVT#
69
#AST#
43
#ART#
50