J Dent Res:血清淀粉样蛋白A通过TLR2和TLR4促进慢性根尖周炎的发生
2018-09-22 lishiting MedSci原创
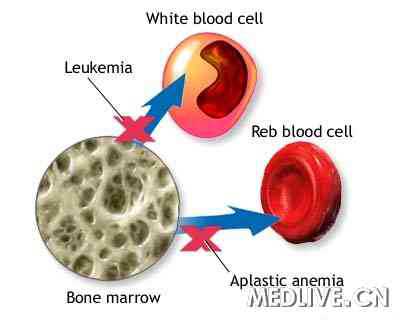
在现代细菌感染理念中,一直认为来源于病原体的病原相关分子模式(PAMPs)和来源于损伤/坏死宿主细胞的损伤相关分子模式(DAMPs)是诱导固有免疫反应的主要因素。然而,DAMPs在根尖周炎及边缘牙周炎中的作用还未可知。血清淀粉样蛋白A (SAA)是一种DAMP,它涉及多种慢性炎症性疾病的发展,如风湿性关节炎。在这篇研究中,作者利用人的尖周手术样本以及SAA和Toll-like receptors
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#TLR2#
68
#TLR#
48
#根尖周炎#
51
#TLR4#
52
#淀粉样蛋白#
41