Neurol Neuroimmunol Neuroinflamm: 结构和功能MRI网络可预测多发性硬化症临床恶化
2021-06-23 MedSci原创 MedSci原创
该研究发现整合结构和功能MRI网络措施改善了对临床恶化的预测。
多发性硬化(MS)是最常见的炎症、脱髓鞘和神经退行性中枢神经系统疾病,具有很大的个体间差异性。现在有几种疾病改变疗法(DMTs)可用,2有越来越多的需求来识别有更严重的疾病演变的MS患者,以优化患者的管理和增加获益/风险比。
传统的MRI革新了多发性硬化症的评估,并正式纳入多发性硬化症的诊断标准。在治疗的多发性硬化症患者中,MRI疾病活动性指标与临床评价相结合,以指导治疗决策。然而,常规MRI对后续病程的预测价值仍存在争议,只有一些研究发现白质(WM)病变负荷对疾病发展有显著影响。
在多发性硬化症(MS),临床损伤可能是由于结构损伤和大脑功能异常。最近,Neurol Neuroimmunol Neuroinflamm杂志发表研究文章,评估了结构和功能网络MRI测量预测6.4年MS临床残疾恶化的价值。

该研究假设整合结构和功能网络信息可能有助于识别对异质性疾病(如MS)的临床恶化至关重要的特定回路,并可能改善对随后病程的预测,尤其在残疾方面增加和演变为更严重的临床表型。为了验证这一点,该研究分析了来自一个大型MS队列的体积和RS功能磁共振数据,并绘制了主要数据驱动的功能和结构GM网络的异常。然后,在6.4年的随访中,评估了结构和功能网络MRI测量预测临床残疾恶化和继发性进展(SP) MS的附加价值。
233例MS患者和77例健康对照者的基线3D T1加权和静息状态功能MRI扫描结果。患者在基线和6.4年的中位随访时进行了神经学评估(四分位数范围= 5.06-7.51年)。随访时,根据残障改变将患者分为临床稳定/恶化。在复发-缓解(RR) MS中,评估继发性进展(SP) MS的转化。获得全脑体积测量结果。此外,通过独立分量分析确定了主要功能连接(FC)和灰质(GM)网络模式。
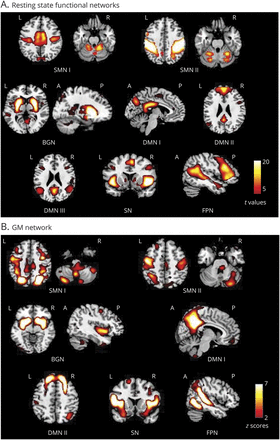
多发性硬化症(MS)患者和健康对照组(HC)患者与感觉、运动和高阶整合功能相关的主要功能和结构感兴趣网络。相关(A)静息态(RS)功能连接(FC)和(B)灰质(GM)网络的空间图。RS FC网络设置阈值p<0.05,FEW校正。通过视觉检查和与RS FC网络的空间匹配选择GM结构网络,并在之前的研究中使用阈值z-scor>2。
随访时,105/233例(45%)患者出现临床恶化;26/157 (16%) RRMS患者演变为SPMS。治疗调整随机森林模型确定了标准化GM和脑容量,减少了默认模式网络之间的FC,增加了左侧中央前回的感觉运动网络(SMN)的FC,额顶叶网络中的GM萎缩(假发现率[FDR]校正p =范围0.01-0.09)作为临床恶化的预测因子(袋外[OOB]准确性= 0.74)。基线残疾的预期贡献也存在(FDR-p = 0.01)。SMN中基线功能障碍、标准化GM体积和GM萎缩(FDR-p =范围0.01-0.09)与SPMS转换独立相关(OOB准确性= 0.84)。在受试者工作特征分析中,包括网络MRI变量改善了残疾恶化(p = 0.05)和SPMS转换(p = 0.02)预测。

HC和MS功能和结构网络的组间比较。(A) RS FC的体素组间比较:蓝-浅蓝色标度显示RS FC在MS vs HC中下降,而红-黄色标度显示RS FC在MS vs HC中增加(年龄和性别校正的两样本t检验,p<0.001为未校正)。(B)显示相关GM网络的平均加载系数(均值和SDs)的箱线图。
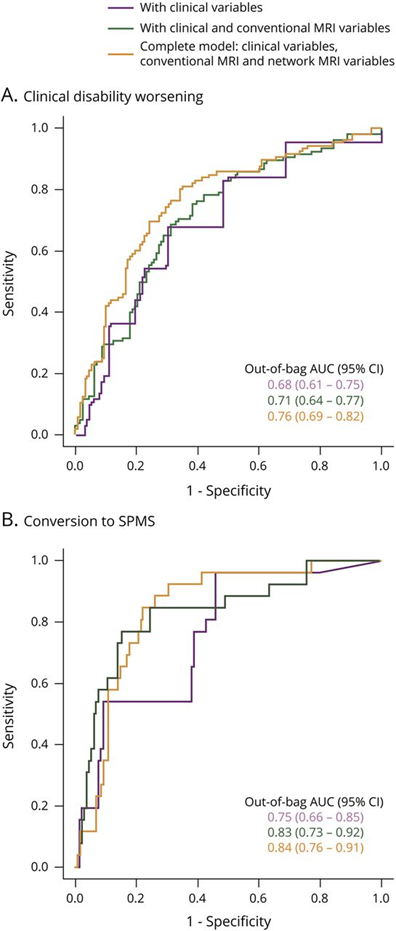
分析预测。ROC分析结果显示曲线下的面积(OOB AUC)随机森林模型预测临床残疾恶化(A)转换为SPMS(B)。模型显示相关联的AUC的增量的包含常规MRI变量(绿线)和网络MRI变量(橙色线)除了混杂协变量和临床变量(紫色线)。
通过对一组有6.4年随访的MS患者进行分析,发现整合结构和功能网络措施显著改善了临床恶化预测。除了较高的基线EDSS评分和较低的全GM体积,感觉运动和DMNs内部和之间的RS FC基线异常,以及感觉运动和认知GM网络萎缩,有助于解释整体残疾进展。此外,SMN中GM萎缩是SPMS转化的决定因素之一。
总之,该研究发现整合结构和功能MRI网络措施改善了对临床恶化的预测。其它MRI和血清学生物标志物的附加价值可能是未来研究的主题,如通过弥散加权MRI评估WM网络损伤,通过磁化转移成像获得的脱髓鞘/再髓鞘指数,或神经丝轻链。
原文出处
Network Damage Predicts Clinical Worsening in Multiple Sclerosis:A 6.4-Year Study. Maria A. Rocca, Paola Valsasina, Alessandro Meani, Elisabetta Pagani, Claudio Cordani, Chiara Cervellin, Massimo Filippi. Neurol Neuroimmunol Neuroinflamm Jul 2021, 8 (4) e1006; DOI: 10.1212/NXI.0000000000001006
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言











#Neurol#
51
#临床恶化#
51
#LAM#
65
#多发性#
49
#硬化症#
57
#NFL#
47