JACC:ST段抬高心肌梗死患者的循环酮体水平越高,预后可能越差!
2021-10-10 Nebula MedSci原创
ST段抬高心肌梗死患者的循环酮体水平越高,预后可能越差!
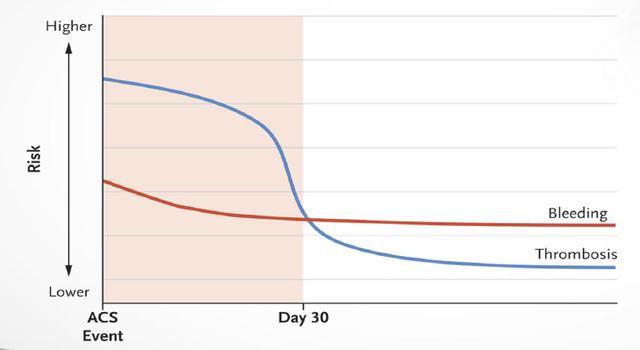
虽然在过去数十年里,心肌梗死(MI)的发病率和死亡率都有明显降低,但心肌梗死仍是发展成心力衰竭(HF)的重要风险因素。酮体(KB)是心力衰竭时心肌代谢的主要细胞能量来源。
既往研究发现,心力衰竭患者的循环酮体水平升高,对应了心脏酮体代谢增加和心力衰竭的严重程度。但是,迄今为止,循环酮体在心肌缺血/再灌注中的作用仍未明确。
本研究旨在调查酮体的纵向变化及其与 ST 段抬高型心肌梗死 (STEMI) 患者功能预后的相关性。
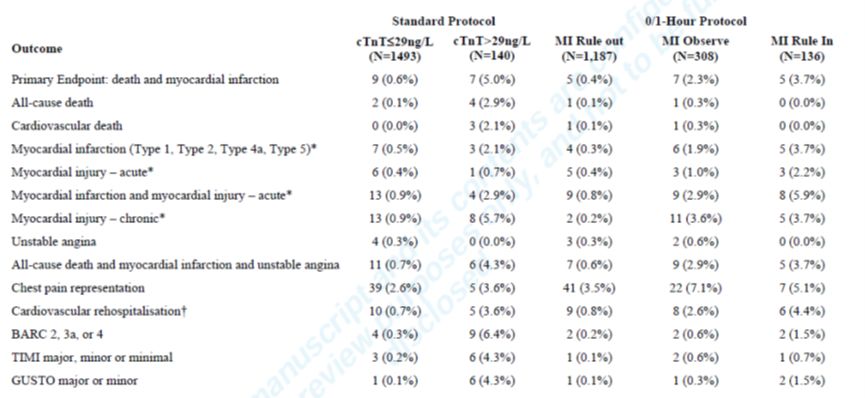
研究人员检测了来自关于 STEMI 后早期应用二甲双胍的随机试验的 369 位受试者的循环酮体。分别在就诊时、24 小时和 4 个月后,通过核磁共振波谱测量了酮体(β-羟基丁酸、乙酰乙酸和丙酮)的非空腹血浆浓度。在 4 个月时通过心脏磁共振成像确定心肌梗死面积和左心室射血分数 (LVEF) 。采用多变量线性回归分析确定循环酮体与心肌梗死面积和 LVEF 的关联。
不同时间点的酮体水平
在 STEMI 出现时,循环酮体水平升高(总酮体的中位水平:520 μmol/L)。与随访 4 个月时的酮体水平相比,再灌注后 24 小时时的酮体水平仍然很高(206 μmol/L vs 166 μmol/L,p<0.001)。24 小时时的酮体水平升高与更大的心肌梗死面积(总酮体,每 100 μmol/L: β=1.56; 95% CI 0.29~2.83; p=0.016)和更低的 LVEF (β=-1.78; 95% CI -3.17~-0.39; p=0.012)相关。
酮体水平与功能预后的相关性
总而言之,STEMI 患者的循环酮体水平升高。24 小时时较高的酮体水平与患者 STEMI 后的功能预后相关,提示酮体代谢可能参与机体对心肌梗死的应答反应。
原始出处:
de Koning Marie-Sophie L Y,Westenbrink B Daan,Assa Solmaz et al. Association of Circulating Ketone Bodies With Functional Outcomes After ST-Segment Elevation Myocardial Infarction.[J] .J Am Coll Cardiol, 2021, 78: 1421-1432.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#JACC#
93
#ACC#
69
#ST段抬高#
99
#ST段抬高心肌梗死#
64
#ST段#
87
我都要走了么铝模路线
129
值得关注
89
#高血压#值得学习
108
涨知识了
104