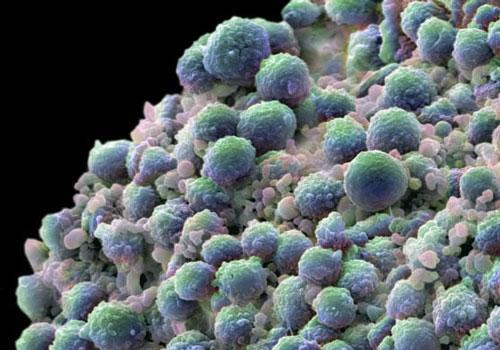
Oncotarget:循环miRNA可用于卵巢癌的早期精准筛查
2017-12-03 MedSci MedSci原创
由于早期发现困难,卵巢癌是导致妇科恶性肿瘤死亡的主要原因。目前的筛查方法准确性不足,仍缺乏一种新的早期检测方法,以较小的损伤改善患者的预后。尽管许多研究表明循环microRNA在癌症检测中的作用,但其在卵巢癌早期发现的方面的应用仍尚未清楚。本研究中,研究人员使用8种循环血清miRNAs开发新的预测模型。该方法成功地将卵巢癌患者与良性对照组(曲线下面积,0.97,敏感性,0.92,特异性,0.91)
由于早期发现困难,卵巢癌是导致妇科恶性肿瘤死亡的主要原因。目前的筛查方法准确性不足,仍缺乏一种新的早期检测方法,以较小的损伤改善患者的预后。尽管许多研究表明循环microRNA在癌症检测中的作用,但其在卵巢癌早期发现的方面的应用仍尚未清楚。
本研究中,研究人员使用8种循环血清miRNAs开发新的预测模型。该方法成功地将卵巢癌患者与良性对照组(曲线下面积,0.97,敏感性,0.92,特异性,0.91)以及良性肿瘤患者与早期卵巢癌区分开来(分别为0.91,0.86和0.83)。此外,该方法还可用于4种上皮性卵巢癌的亚型分类。进一步研究发现,8个miRNAs中大部分存在来源于卵巢癌细胞细胞的外囊泡中,包括外泌体,并存在小鼠的血液循环中。
综上所述,本研究结果表明,所选用的8种循环miRNAs可作为检测卵巢癌患者的生物标记物。术前的早期发现和亚型鉴别是医生为每位患者制定个性化有效治疗策略的关键,这也是精确医学的目标。
原始出处:
Yokoi A, Yoshioka Y, et al., A combination of circulating miRNAs for the early detection of ovarian cancer. Oncotarget. 2017 Sep 6;8(52):89811-89823. doi: 10.18632/oncotarget.20688. eCollection 2017 Oct 27.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#miR#
44
#target#
45
很好
86
#miRNA#
52
#精准#
45