BMJ:阿托伐他汀对ICU新冠肺炎重症患者预后的影响
2022-01-10 MedSci原创 MedSci原创
在ICU收治的重症Covid-19成人患者中,接受阿托伐他汀治疗不能降低患者血栓、接受体外膜氧合治疗或全因死亡风险,对改善患者预后无显著效果

Covid-19可导致多个靶器官异常,过度活跃的免疫反应可导致肺和肺外损伤,其中肺实质损伤是重症Covid-19患者最常见、最危险的特征,可发展为急性呼吸窘迫综合征。在血管内皮激活条件下,重症患者的微血栓和大血栓风险增加,其中ICU中静脉血栓的发病率及死亡率极高。羟甲基戊二酰辅酶A还原酶抑制剂,主要是他汀类药物,具有抗炎和抗血栓形成的作用。他汀类药物可通过抑制NF-kB通路,减少炎症反应,此外他汀类药物也具有抗氧化和抗凋亡的作用。近日研究人员评估了他汀类药物对重症监护病房(ICU)收治的Covid-19患者临床结局的影响。
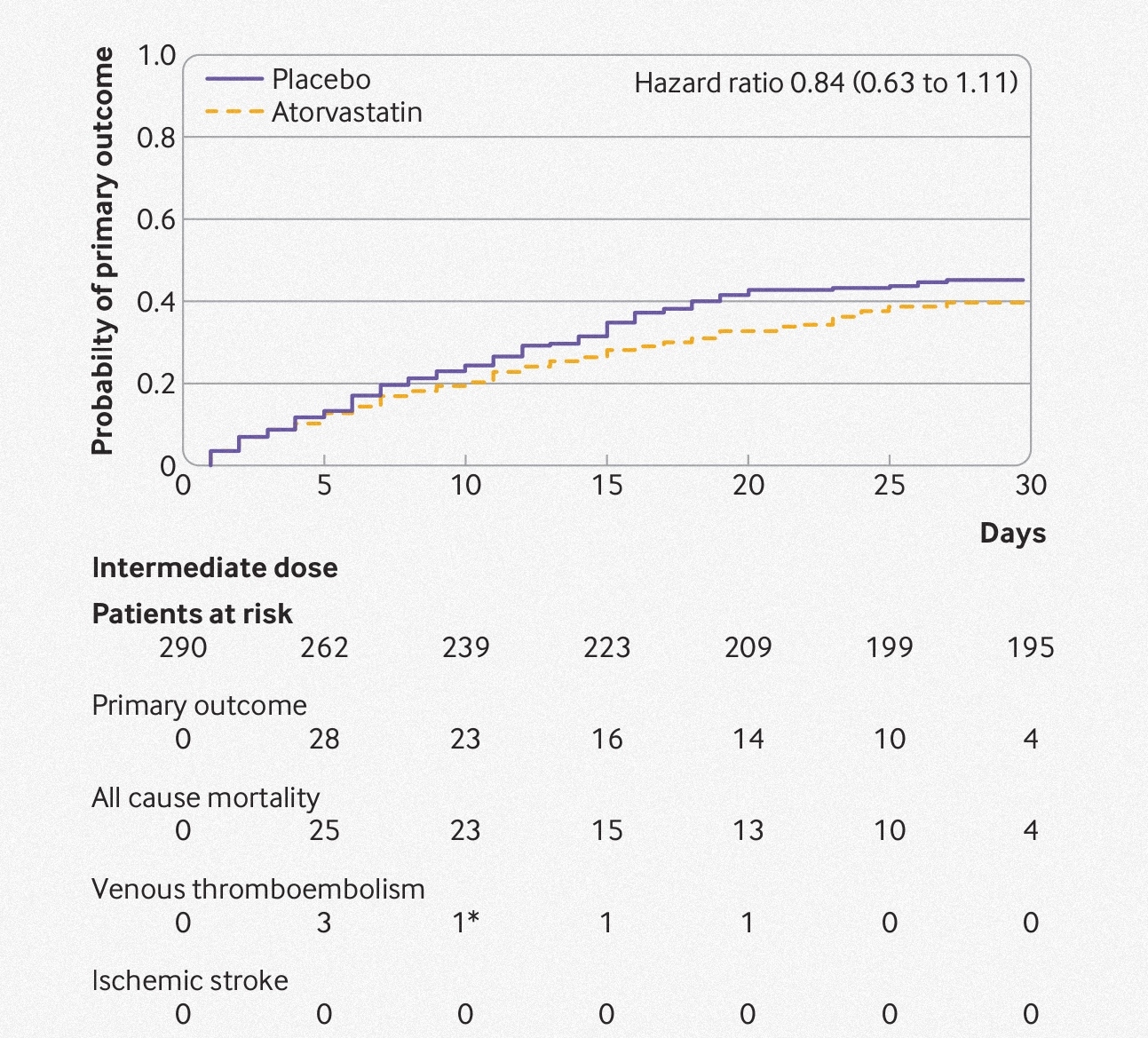
INSPIRATION/INSPIRATION-S是一项多中心随机对照试验,在伊朗11家医院开展,收入ICU治疗的Covid-19成年患者参与,患者随机接受每日1次,每次20mg的阿托伐他汀治疗或安慰剂,持续30天。主要疗效终点是静脉或动脉血栓、体外膜肺氧合治疗或随机分组后30天内死亡。安全性终点包括肝酶水平超过上限三倍或肌病。
587名患者参与研究,其中阿托伐他汀组290人,安慰组297人,患者平均年龄57岁,女性256人(44%)。阿托伐他汀组95名(33%)患者出现主要终点事件,安慰剂组108名(36%,比值比0.84)。阿托伐他汀组有90名(31%)患者死亡,安慰剂组有103名(35%)患者死亡(风险比0.84)。阿托伐他丁组静脉血栓栓塞率为2%(n=6),安慰剂组为3%(n=9,风险比0.71)。参与者中未出现肌病,但阿托伐他汀组的5名(2%)患者和安慰剂组的6名(2%)患者的肝酶水平升高(优势比0.85)。
阿托伐他汀治疗对患者预后的影响
研究发现,在ICU收治的重症Covid-19成人患者中,接受阿托伐他汀治疗不能降低患者血栓、接受体外膜氧合治疗或全因死亡风险,对改善患者预后无显著效果。
原始出处:
INSPIRATION-S Investigators. Atorvastatin versus placebo in patients with covid-19 in intensive care: randomized controlled trial. BMJ,07 January,2022。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#BMJ#
58
#患者预后#
68
学习了
80
厉害
81
#重症患者#
70