JNNP:抑郁症患者REM睡眠行为障碍的患病率及其相关因素
2021-11-14 MedSci原创 MedSci原创
影响全球近3亿人的抑郁症已成为全球第三大致残原因。有人认为,“晚发性”抑郁症更可能与神经退行性变的未来风险相关。需要一种更具体的特征或/和生物标记物来识别和治疗这种神经退行性变
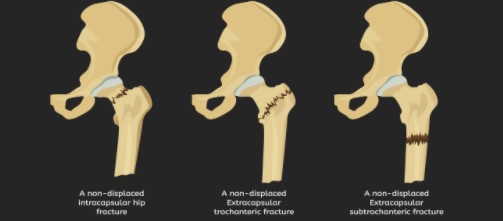
影响全球近3亿人的抑郁症已成为全球第三大致残原因。有人认为,“晚发性”抑郁症更可能与神经退行性变的未来风险相关。需要一种更具体的特征或/和生物标记物来识别和治疗这种神经退行性变相关抑郁症亚型。快速眼动(REM)睡眠行为障碍(RBD)是一种新型的嗜睡障碍,其特征是反复的做梦行为导致重复的睡眠相关发声/运动行为和睡眠相关损伤(SRI),并伴有REM睡眠中的肌肉张力丧失。

90%以上的特发性RBD(iRBD)患者会发展为α-突触核蛋白病神经退行性变,其中大多数是帕金森病(PD)和路易体痴呆(DLB)。RBD在普通人群中的患病率约为1%。RBD特征出现在精神病人群中,尤其是重度抑郁症(MDD)患者。通过使用最近1年的SRI史作为RBD症状的替代项目,之前估计精神科门诊患者RBD的终生患病率为5.8%(MDD亚组为6.8%)。然而,vPSG在MDD患者(MDD+RBD)中证实RBD的真实患病率可能被低估。通过验证筛查问卷和vPSG确认,本研究进行了这项两阶段研究,以(1)确定MDD+RBD的患病率;(2)研究MDD+RBD患者的临床相关性,尤其是神经退行性变的风险。本文发表在《神经病学,神经外科学和精神病学杂志》上()。

香港RBD问卷(RBDQ-HK)是一份包含13个项目的问卷,包含终生和最近1年的子量表,涵盖RBD中的梦相关因素和行为因素。先前的验证研究表明,诊断精神病患者RBD的临界值为20/21。共有302名患者同意进行进一步的临床评估,其中,精神病诊断通过DSM-IV轴I疾病的结构化临床访谈确定。抑郁症的严重程度和非典型症状使用汉密尔顿抑郁评定量表(SIGH-ADS)的结构化访谈威廉亚洲博彩公司 进行评估由经验丰富的精神病医生进行。患者还完成了与睡眠、生活方式因素和接触史(如头部受伤)相关的额外问卷调查。相关的医疗信息是在一个完善的电子医疗数据库中获得的。
研究流程图
筛查阳性(RBDQ-HK>20)患者以及随机选择的部分筛查阴性患者被邀请参加睡眠实验室vPSG评估的第2阶段研究。根据美国睡眠医学学会标准(2012年)对睡眠阶段、呼吸事件、觉醒和运动事件进行评分在RSWA的允许下,13名患者被要求在研究期间继续他们的常规药物治疗。如果出现显著的呼吸暂停/低通气事件(呼吸暂停低通气指数≥15) ,患者将被邀请进行第二晚vPSG,滴定持续气道正压,第二晚vPSG数据将用于评分。REM睡眠时下巴肌肉上的肌电图(EMG)活动水平用于确定RSWA的严重程度,因为建议下巴肌电图提供最高的阶段性EMG活动。
在不同领域测量与RBD和神经退行性变相关的危险因素和前驱标记物。使用帕金森病自主神经功能障碍(SCOPA-AUT)量表中的结果量表测量自主神经功能障碍症状,并在仰卧位站立2分钟内(休息5分钟后)进一步测量立位血压变化。采用最新的运动障碍学会(MDS)研究标准来估计前驱症状PD的总似然比(LR)和概率。RBD的诊断是根据国际睡眠障碍分类第三版标准进行的。在睡眠医学方面经验丰富的精神科医生通过对睡眠模式和障碍23的诊断性访谈和病例注释审查,澄清了RBD反复出现的做梦行为症状。
第一阶段,接触了751名抑郁症患者,其中504名(平均年龄49.85岁,77.0%为女性,应答率67.1%)同意本研究。在诊断访谈和医疗记录审查后,48名患者因发作性睡病(n=1)、中风(n=1)、创伤后应激障碍(n=16)、药物滥用(n=11)、双相情感障碍(n=17)和终身未诊断MDD(n=2)而被排除在外。一名患者因未完成RBDQ-HK而被排除在外。其余455名符合条件的MDD患者(中位年龄(IQR)=52.66(15.35)岁,77.58%为女性)被确定为全筛查样本。其中302名患者(54.04(13.12)岁,76.49%为女性)完成了额外的问卷调查和临床访谈,并被视为样本总数。
伴和不伴RBD的重度抑郁症患者的对数总似然比(LR)
筛查阳性患者包括更多的吸烟者(14.39%比7.36%),更有可能报告头部损伤史(12.23%比6.13%),但在调整人口统计学后,差异变得不显著。筛查阳性患者也表现出更严重的抑郁症状(汉密尔顿抑郁评分量表17项评分),比其对应患者更非典型的抑郁特征(4.00(4.00)vs 3.00(4.00))。此外,筛查阳性患者白天嗜睡率较高,失眠率可能较高。共有81名患者(54.08(12.40)岁,65.43%为女性,51名筛查阳性)完成了vPSG和神经认知评估。8名男性和4名女性筛查阳性MDD患者(即MDD+RBD,RBD发病年龄=53(11)岁,3名患者在开始服用抗抑郁药之前报告RBD发病)证实RBD,其余69名患者被归类为非RBD。MDD+RBD的加权患病率为8.77%。MDD+RBD与色觉和嗅觉缺陷以及PD的高度相关。
总之,在精神科门诊部,几乎9%的MDD患者有vPSG证实的RBD。共病MDD+RBD可能是MDD的一个亚型,伴有潜在的α-突触核蛋白病神经退行性变。应强调RBD症状的系统筛查和vPSG确认的必要性,以识别这种MDD亚型,从而加强个性化治疗和未来的神经保护,以防止神经退行性变。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言

















#抑郁症患者#
80
#行为障碍#
83
#患病率#
145
#相关因素#
113
#REM#
83