ACC 2022:二叶式主动脉瓣和三叶式主动脉瓣反流结局却大不相同!
2022-04-15 网络 网络
与BAV-AR相比,TAV-AR患者处于AR过程的后期,AD率较高,强调了早期治疗的重要性。
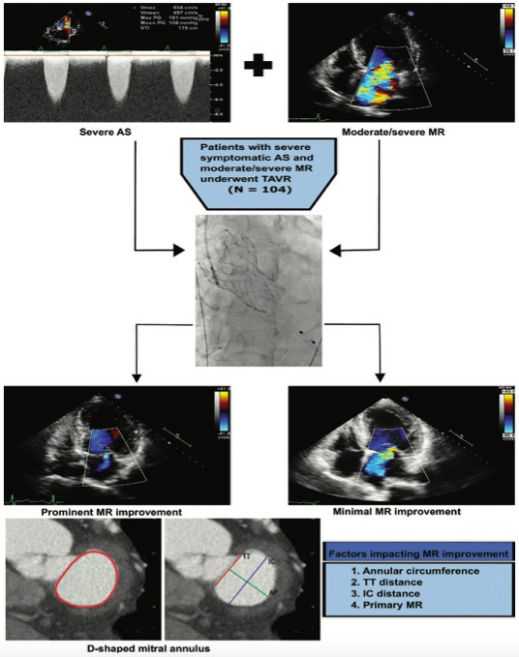
经导管主动脉瓣置换术(transcatheter aortic valve replacement,TAVR),又称经导管主动脉瓣置入术(transcatheter aortic valve implantation,TAVI),是指将组装完备的人工主动脉瓣经导管置入到病变的主动脉瓣处,在功能上完成主动脉瓣的置换。自2002年首例成功以来,TAVR已成为老年主动脉瓣狭窄(aortic stenosis,AS)患者的一线治疗手段。欧美国家相继颁布并更新了TAVR的指导性文件。我国TAVR发展相对缓慢,2010年10月3日开展了首例TAVR。但自2017年两款国产瓣膜上市以来,我国TAVR进入快速、全面发展阶段。
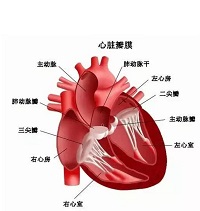
心脏内有四个瓣膜,可以保持血液的流动方向正确。这些瓣膜包括二尖瓣、三尖瓣、肺动脉瓣和主动脉瓣。每个瓣膜都有瓣叶(小叶或尖头),心脏每跳动一次,这些瓣叶就会打开和关闭一次。有时候,瓣膜无法正常打开或关闭,这将阻碍血液从心脏流向身体。
当症状较轻时,瓣膜反流通常不会引起任何问题。但是,重度瓣膜反流可能引起并发症,包括心衰、房颤、肺动脉高压及主动脉并发症等。
在西方国家,AS是老年人群常见心脏疾病,其发病率随着年龄增长逐渐增高,在年龄≥65岁人群中约占2.0%,在≥85岁人群中约占4%。我国尚无AS确切流行病学数据。一项单中心超声心动图数据库分析提示我国AS发病率可能低于国外。其他一些间接性的调查研究显示,相对于西方国家,我国TAVR候选患者和西方国家存在一些差异:二叶式主动脉瓣(bicuspid aortic valve,BAV)比例较高、主动脉瓣钙化程度较高、主动脉瓣反流(aortic regurgitation,AR)多于AS、风湿性病因比例高、股动脉内径较细。在接受TAVR的BAV患者各解剖亚型的构成比中,我国患者0型(无嵴型)占比较西方国家高。虽然我国TAVR候选人群中BAV的比例较高,但是,一项单中心研究显示,我国重度AS患者中BAV的比例(60~80岁约为50%,≥80岁约为20%)可能与国外接近。另外一项基于超声心动图数据库大样本人群分析显示,我国BAV发病率及并发症发生率与西方人群接近。
基于PARTNER2研究及SURTAVI研究的结果,目前欧美威廉亚洲博彩公司 已将外科手术极高危、高危及中危患者列为TAVR的适应证。2019年美国心脏病学会(American College of Cardiology,ACC)公布了低危患者TAVR的研究包括PARTNER 3研究(使用球扩式瓣膜Sapien 3)和Evolut Low Risk Trial研究(使用自膨式瓣膜Evolut R),显示外科手术低危患者接受TAVR的效果优于或不劣于外科手术。基于这两项研究结果,2019年美国和欧洲政府部门批准Sapien 3及Evolut R人工瓣膜应用于外科手术低危患者。截至2019年底,国外已有十几种TAVR瓣膜获批上市应用于临床,全球共完成超过40万例TAVR。
2017年5月,两款国产瓣膜(Venus-A和J-Valve)获批上市;2019年7月另一国产瓣膜(VitaFlow)获批上市。Venus-A瓣膜、VitaFlow瓣膜为经外周动脉逆行入径的自膨式瓣膜。J-Valve为经心尖入径瓣膜,可治疗AS和AR。国产瓣膜的上市,推动了我国TAVR的快速发展。截至2019年底,全国已有20多个省市、约200家医院共完成4000余例TAVR,其中2019年完成了2600多例。我国在TAVR方面积累了自己的经验。目前从我国几大中心经验看来,BAV和三叶式主动脉瓣(tricuspid aortic valve, TAV)的TAVR效果比较,差异无统计学意义。J-Valve瓣膜具有锚定装置,适合于AR患者的治疗。我国在AR患者的TAVR治疗方面积累了较多经验。总体上,我国TAVR累计完成数量小,具有独立开展TAVR能力的中心少,较国外有一定差距,患者临床特点也与国外患者存在差异。
亚洲人口在不断增长,但有关主动脉瓣反流(AR)的二叶式主动脉瓣(BAV)和三叶式主动脉瓣(TAV)之间的差异的亚洲数据仍未得到探索。为了研究亚洲人二叶式主动脉瓣(BAV)-AR和三叶式主动脉瓣(TAV)-AR在显著的AR方面的差异,来自我国宝岛台湾的专家开展了相关研究,结果发表在近期ACC2022学术大会上。
研究人员在2008年至2020年连续纳入711名慢性≥中度-重度AR患者。结果包括全因死亡、主动脉手术(AVS)和主动脉夹层(AD)的发生率。
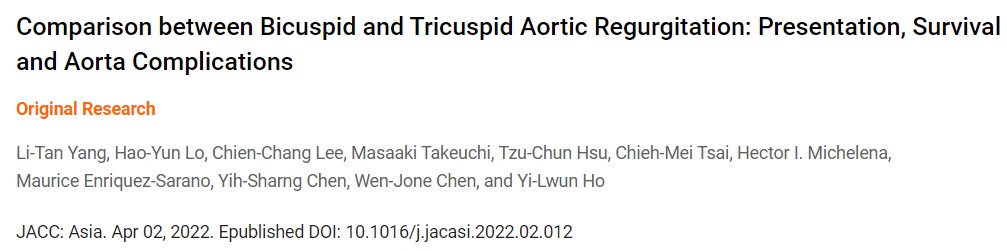
结果显示,有149名BAV-AR(年龄48±16岁)和562名TAV-AR(年龄68±15岁)患者;TAV-AR的基线左心室指数和主动脉直径更大。总随访时间为4.8(IQR:2.0-8.4)年,252例接受了AVS,185例在随访期间死亡;18例(仅1例BAV)发生AD,平均最大主动脉尺寸为60±9mm。
即使在调整了协变量后,TAV-AR的10年AVS-发病率(51±4%)高于BAV-AR(40±5%)。BAV-AR的10年生存率(86±4%)高于TAV-AR(57±3%)。BAV-AR和TAV-AR的10年生存率分别为93±5%和78±5%(P=0.08)。TAV-AR的10年发病率(4.8±1.5%)高于BAV-AR(0.9±0.9%),且由主动脉≥45mm决定。与年龄和性别匹配的人群相比,TAV-AR(HR=3.1)的生存率降低。
综上,研究结果表明,与BAV-AR相比,TAV-AR患者处于AR过程的后期,AD率较高,强调了早期治疗的重要性。
参考文献:
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言














#主动脉瓣反流#
66
#二叶式主动脉瓣#
57
#ACC#
54
#主动脉瓣#
62
#主动脉#
66
#反流#
68