BMJ Open:长期使用睡眠药物或不能改善睡眠质量
2021-05-12 MedSci原创 MedSci原创
据统计,我国有超过3亿人存在睡眠障碍,成年人失眠发生率达38.2%,六成以上的90后觉得睡眠不足,失眠成为了现代人的“新”流行病。
据统计,我国有超过3亿人存在睡眠障碍,成年人失眠发生率达38.2%,六成以上的90后觉得睡眠不足,失眠成为了现代人的“新”流行病。

CCO
很多失眠者选择服用药物,近日发表在BMJ Open杂志的一项研究却显示,长期使用处方药治疗失眠似乎并不能改善中年女性的睡眠障碍,在服用和未服用失眠药物人群中,睡眠质量并没有差异。

该研究共纳入来自《全国妇女健康研究》(SWAN)238名开始服用睡眠药物的女性与447名未使用药物女性。参加者的平均年龄为49.5岁,大约一半是白人。睡眠障碍的定义为入睡困难,频繁唤醒和及早起床,并以5分制进行评分。同时,根据评分量表对睡眠障碍进行了比较,使用和不使用处方药参与者在1年和2年后对睡眠是否有影响。
结果显示,在基线时,两组女性的睡眠障碍评分相似。药物使用者的平均入睡困难评分为2.7(95%CI 2.5至2.9),经常醒来为3.8(95%CI 3.6至3.9)和清晨醒来为2.8(95%CI 2.6至3.0)。未使用药物者评分分别为2.6(95%CI 2.5至2.7),3.7(95%CI 3.6至3.9)和2.7(95%CI 2.6至2.8)。
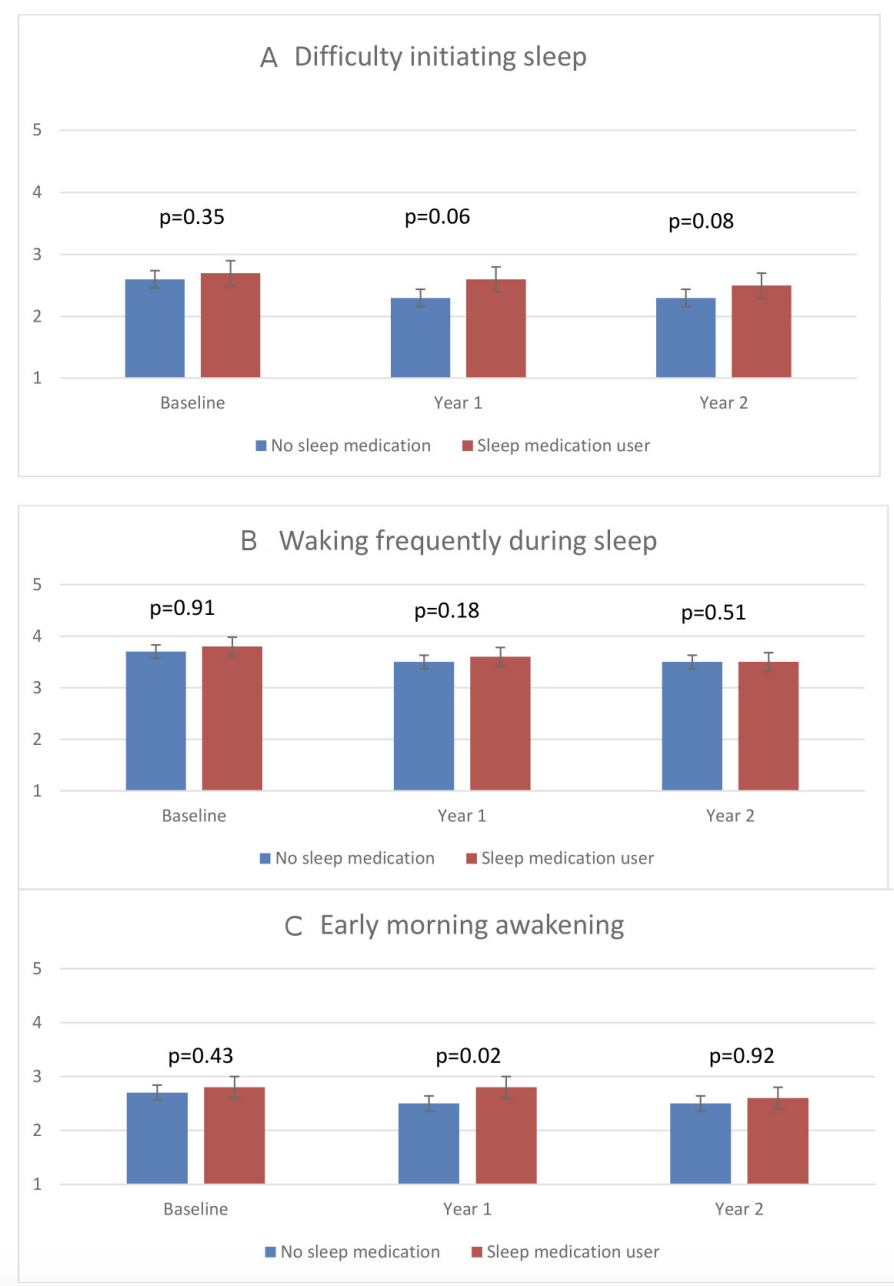
睡眠药物暴露的睡眠障碍评分等级.
一年后,用药使用者平均入睡困难评分为2.6(95%CI为2.4至2.8),经常醒来的评分为3.6(95%CI为3.4至3.8),清晨醒来的评分为2.8(95%CI为2.6至3.0)。对于未使用药物者,平均评分分别为2.3(95%CI 2.2至2.5),3.5(95%CI 3.3至3.6)和2.5(95%CI 2.3至2.6)。两组的1年变化均无统计学意义,也无差异。2年后,与未使用处方药的人相比,使用处方药者的睡眠障碍没有统计学差异。

从基线到第1年和第2年,参与者自我报告的睡眠障碍情况.
研究人员表示,该研究为观察性研究,无法确定其中因果关系,只能建立关联。而且大约一半的女性是现在或以前的吸烟者,五分之一的女性是中度至重度饮酒者,这两个因素都可能影响睡眠质量。尽管相对缺乏RCT的证据,但睡眠药物的使用已经增长,并且经常被长期使用。
总之,睡眠障碍很普遍,并且患病率正在增加。当前的观察性研究不支持长期使用睡眠药物,因为将睡眠药物使用者与非使用者进行随访的1或2年没有显著差异。虽然一小部分患有睡眠障碍的患者可能会在几年内从使用睡眠药物中受益,但在研究了1年和2年后的人群中缺乏与使用睡眠药物相关的益处,未来需要更多证据阐明睡眠药物的优势和劣势。
原始出处
Daniel H Solomon et al. Prescription medications for sleep disturbances among midlife women during 2 years of follow-up: a SWAN retrospective cohort study, BMJ Open (2021). DOI: 10.1136/bmjopen-2020-045074
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#长期使用#
67
#PE#
59
#BMJ#
52
学习,
77
#睡眠质量#
53