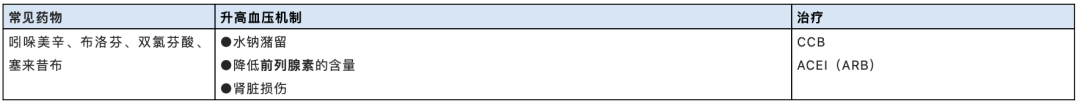
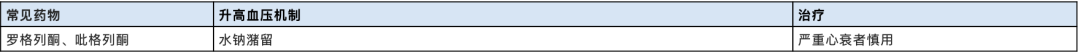
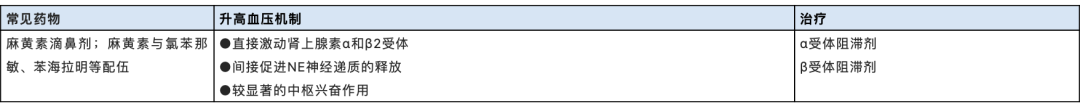
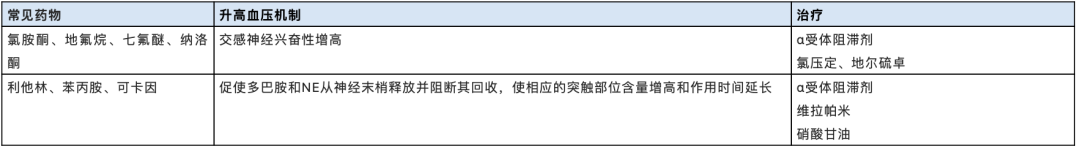
药物性高血压是常规剂量的药物本身或该药物与其他药物之间发生相互作用而引起血压升高,当血压>140/90mmHg时即考虑药物性高血压。原则上,一旦确诊高血压与用药有关,应该尽量停用这类药物,换用其他药物或者采取降压药物治疗。 01 甘草类 温馨提示: 前列腺素和组胺有扩血管作用。甘利欣(甘草酸二铵):主要用于伴有谷丙氨基转移酶升高的急、慢性病毒性肝炎的治疗。生胃酮(甘珀酸钠,甘草次酸的半琥珀酸酯二钠盐):用于消化性溃疡的治疗。 02 非甾体抗炎药 温馨提示: 非甾体抗炎药可减弱降压药的作用。对于一些肾功能不全的病人,血管紧张素转换酶抑制剂与非甾体类抗炎药合用时,可能导致肾功能进一步减退。 03 噻唑烷二酮类降糖药 温馨提示: 罗格列酮:水肿发生率为4.8%,与胰岛素合用时为15.3%。噻唑烷二酮类药物有导致或加重充血性心力衰竭的危险。 04 麻黄素类 温馨提示: 建议高血压和心脏病患者应在医生指导下使用含麻黄的中成药。 05 β2受体激动剂 温馨提示: β2受体激动剂主要用于哮喘,常见不良反包括震颤、头痛、心动过速等。 06 茶碱类 茶碱类可致心律失常,可使原有的心律失常恶化。茶碱与麻黄碱合用可使毒性增强。克林霉素、林可霉素、红霉素、罗红霉素、克拉霉素、依诺沙星、环丙沙星、氧氟沙星等可降低茶碱清除率,增高茶碱不良反应发生率。 07 左甲状腺素 温馨提示: 老年、有心血管疾病患者、有心肌缺血或糖尿病者,应从小剂量开始,给药后应密切观察患者有否心率加快、心律不齐、血压改变。 08 催产素 温馨提示: 垂体后叶素:含催产素和加压素,主要用于肺、支气管出血(如咯血)、消化道出血(呕血、便血),并适用于产科催产及产后收缩子宫、止血等。 09 单胺氧化酶抑制剂类 呋喃唑酮:目前只能用于难以根除的幽门螺旋杆菌感染。利血平:北京降压0号、降压乐等传统复方降压药的成分之一。 10 抗震颤麻痹药 多巴丝肼是左旋多巴与盐酸苄丝肼的复方制剂,也可升高血压。 11 环孢素等免疫抑制剂 12 促红细胞生成素 13 雌激素类 温馨提示: 倍美力(结合雌激素片);内美通(孕三烯酮胶囊);妈富隆(去氧孕烯炔雌醇片)。 14 孕激素类 炔诺酮:用于月经不调、子宫功能出血、子宫内膜异位症等;单方或与雌激素合用能抑制排卵,作避孕药。醋酸甲羟孕酮:可用于月经不调、功能性子宫出血及子宫内膜异位症等。还可用于子宫内膜癌、晚期乳腺癌。 15 雄激素 16 糖皮质激素 17 麻醉药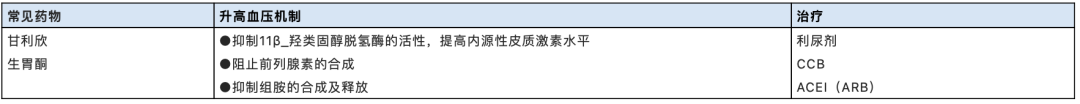
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













学习了
64
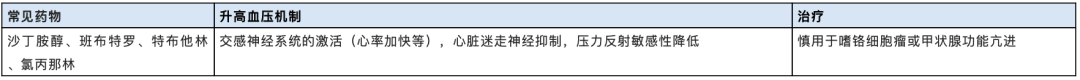
#期刊论坛#来了
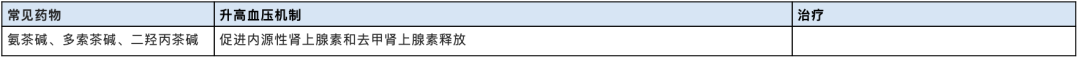
79
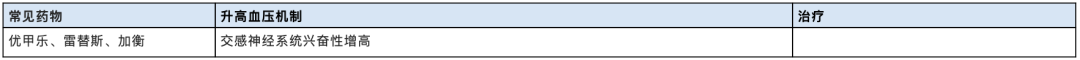
学了
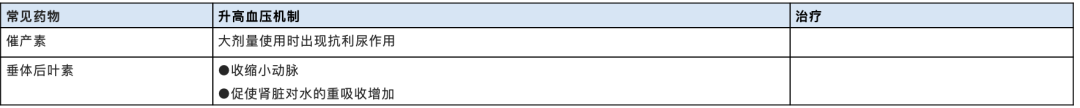
88
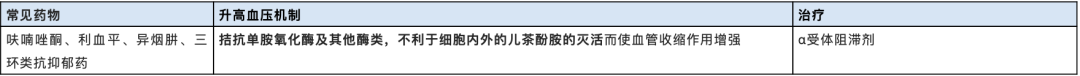
学习
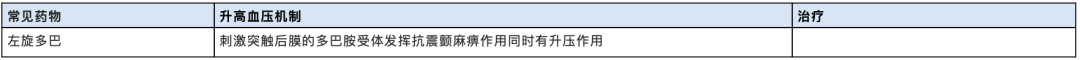
89