2019年美国胸科协会年会:β受体阻滞剂可降低肺移植后房颤的发生率
2019-05-25 不详 网络
根据2019年美国胸科协会年会(ATS)上公布的一项单中心回顾性研究,β受体阻滞剂可降低肺移植后房颤的发生率。
根据2019年美国胸科协会年会(ATS)上公布的一项单中心回顾性研究,β受体阻滞剂可降低肺移植后房颤的发生率。
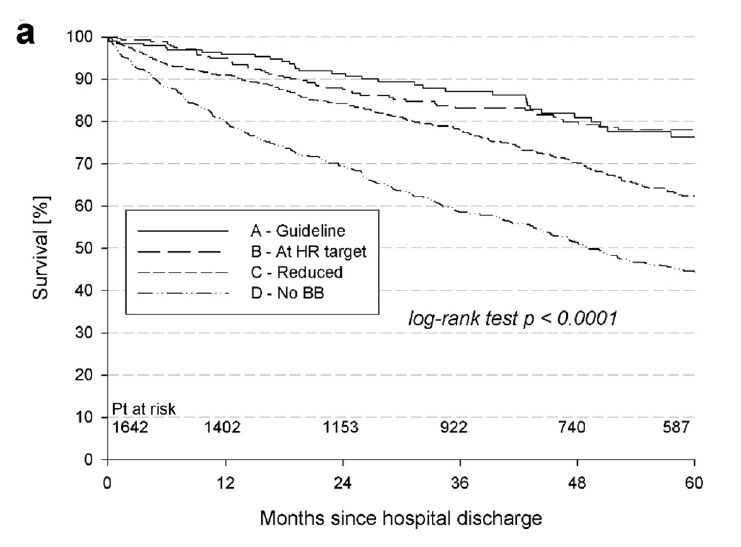
天普大学Lewis Katz医学院Tse-Sheun Jade Ku及其同事对2017年接受肺移植的患者进行了图表审查(n = 116),特别检查了3天内接受美托洛尔以预防房颤(n = 64)的患者。Tse-Sheun Jade Ku博士表示:“接受肺移植且在术后未给予美托洛尔的患者发生原发性房颤的发生率为50%,而接受手术后立即给予美托洛尔的患者,其房颤发生率仅为32.8%(P = 0.06)”。
原始出处:
http://www.firstwordpharma.com/node/1643137#axzz5ovUpnHnX
本文系williamhill asia 医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#阻滞剂#
49
#美国胸科协会年会#
48
#发生率#
56
#受体阻滞剂#
54
#β受体阻滞剂#
51
谢谢分享学习
92