Diabetologia:在2型糖尿病中,IAPP诱导的细胞应激重塑了胰岛转录组
2021-11-18 从医路漫漫 MedSci原创
2型糖尿病胰岛的特征是胰岛淀粉样蛋白来源于胰岛淀粉样肽(IAPP),这是一种由β细胞与胰岛素共表达的蛋白质,当其折叠错误并以聚集形式出现时,可能会导致β细胞衰竭。

2型糖尿病胰岛的特征是胰岛淀粉样蛋白来源于胰岛淀粉样肽(IAPP),这是一种由β细胞与胰岛素共表达的蛋白质,当其折叠错误并以聚集形式出现时,可能会导致β细胞衰竭。人的IAPP (hIAPP)毒性是最有效的介导小的胞内膜渗透寡聚物。具有淀粉样变IAPP的物种,如人类、非人类灵长类动物和猫,都容易患2型糖尿病,而具有非淀粉样变IAPP的物种,如小鼠和大鼠,则不会。虽然已经提出了许多假说来解释2型糖尿病中胰岛的变化,但目前的共识是,在神经退行性疾病中,由有毒淀粉样蛋白低聚物引起的错误折叠蛋白应激引发了这些变化。在本研究中,williamhill asia 评估了糖尿病发病前β细胞hIAPP毒性小鼠模型的胰岛转录组,以避免高血糖的混杂效应。为了控制IAPP表达增加,williamhill asia 评估了小鼠过表达IAPP (rIAPP)的转录组。试图搞清IAPP毒性诱导的胰岛反应是否与2型糖尿病患者的反应相当,如果是,这种反应的关键转录驱动因素是什么?
方法:以12小时的昼夜节律饲养小鼠,hIAPP转基因小鼠在9周龄后发生糖尿病(空腹血糖>6.9 mmol/l),而rIAPP小鼠直到18周龄仍未发生糖尿病,观察结束。只使用9 - 10周龄非糖尿病雄性小鼠。IAPP(内源性和转基因的总和)在rIAPP和hIAPP小鼠中具有可比性。小鼠要么进行空腹血糖测量和GTT代谢研究,要么收集胰岛和胰腺,通过大块胰岛RNA测序(RNA-seq)或qPCR分析RNA。或通过western blotting(在RIPA缓冲液中全细胞裂解液)或免疫染色(在OCT 4%多聚甲醛固定组织中冷冻的4μm厚切片)分析蛋白水平。共分为5组小鼠用来评估胰岛转录组:β细胞特异性转基因(1)人IAPP小鼠,(2)啮齿动物IAPP小鼠,(3)人钙蛋白酶抑制剂,(4)人钙蛋白酶抑制剂和人IAPP小鼠,和(5)野生型小鼠。通过差异表达分析和基因共表达网络分析对RNA测序数据进行分析,以确定胰岛对适应可溶性啮齿动物IAPP增加的β细胞工作量的反应,对寡聚人IAPP增加的表达的胰岛反应,以及后者通过抑制钙蛋白酶抑制素对钙蛋白酶超活化的拯救程度。使用秩-秩超几何重叠分析来比较人或啮齿类IAPP转基因小鼠与糖尿病前期或二型糖尿病人的胰岛转录组。
结果:糖尿病前期和2型糖尿病患者的胰岛转录组非常相似。可溶性啮齿动物或低聚物倾向的人类IAPP的β细胞过表达,导致糖尿病前期和2型糖尿病患者的胰岛转录组发生改变,包括表达β细胞特性的基因减少。增加人类IAPP的表达,而不是啮齿类动物的IAPP,导致出现人类糖尿病前期和2型糖尿病中的胰岛炎症。通过转录因子分析,在转人IAPP或2型糖尿病胰岛中,损伤反应的关键介质包括STAT3、NF-κB、ESR1和CTNNB1,通过基因调控网络分析,包括COL3A1、NID1和ZNF800。
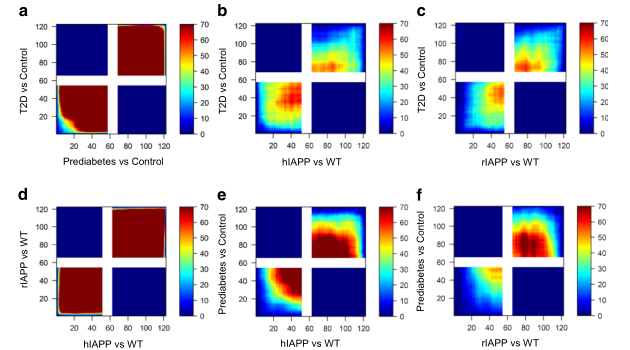
图1 通过RRHO分析评估IAPP在小鼠和人诱导的一致性胰岛转录组变化。像素代表超几何测试(步长= 110)的−log10(p值),并通过彩色编码来可视化重叠的强度和模式。上调基因(信号在左下象限)和下调基因(信号在右上象限)的最大重叠组如图所示。来自糖尿病前期和T2D供体的胰岛的表达谱(相对于正常血糖控制)惊人地相似(a),来自IAPP转基因小鼠模型的胰岛的表达谱(相对于WT,d)也是如此。IAPP转基因小鼠胰岛(相对于WT)的表达谱与T2D (b,c)和糖尿病前期(e,f)人类胰岛的表达谱高度一致。ESM图2列出了经RRHO分析并一致改变的基因比例。T2D, 2型糖尿病
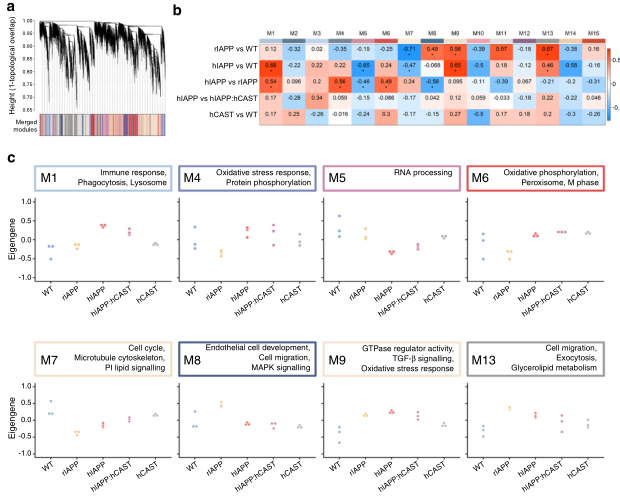
图2 共表达网络的构建与分析。(a)使用所有样本生成的层次聚类树状图,将基因分成15个不同的共表达模块(M1-M15,用颜色标记)。(b)通过拟合基于IAPP和CAST状态的广义线性模型评估模块-性状关系,然后比较基因型对之间的模块特征基因(ME)——相当于一个模块的第一个主成分。采用单向非参数方差分析(one-way, nonparametric ANOVA)和事后Tukey检验(post - hoc Tukey test)检测模块水平的差异表达。ME表达差异以热图表示,其中显著微扰为(*,q< 0.05)。(c)扰动模块轨迹图显示所有样本的归一化表达式
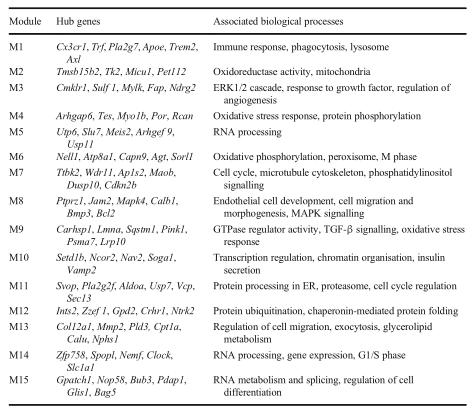
表 共表达模块的功能特征。通过基因集富集分析,选择具有高模内连通性的中枢基因以及与每个模块相关的主要生物学过程
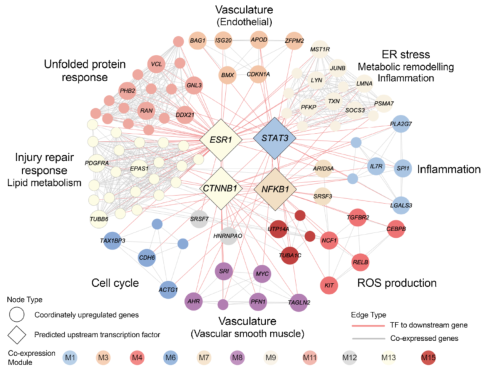
图3 通过RRHO分析确定了在hIAPP和人类2型糖尿病胰岛相对于其各自的对照(WT和非糖尿病人胰岛)中协调上调的基因调控网络。转录因子结合位点富集分析鉴定了过度表达的上游转录因子,包括NF-κ b1,归属于β细胞富集模块(M7),以及STAT3,归属于巨噬细胞和星状细胞标记富集M1的炎症调节关键因子。ESR1和CTNNB1都与β细胞应激/生存信号通路有关。节点颜色反映了共表达式模块的分配。边缘代表实验验证的转录因子-靶标关系(红色)和模内共表达(浅灰色)
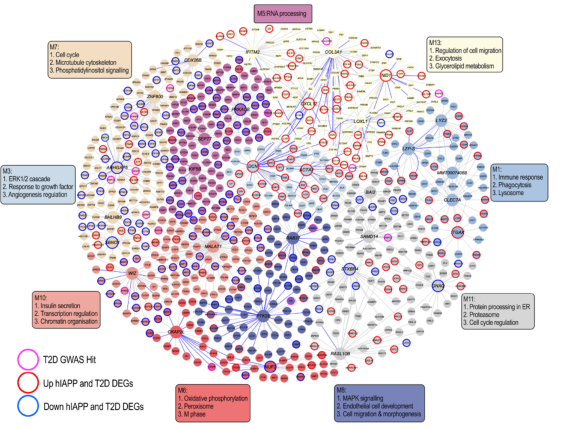
图4 贝叶斯基因调控网络阐明了共表达模块的互连性,并突出了在驱动这些过程中可能重要的关键基因(通过更大的节点大小表示)。T2D GWAS点击率(关联p< 5 × 1 0−8)在网络节点周围以粉红色环突出显示,上调的hIAPP和T2D deg以红色环突出显示,下调的hIAPP和T2D deg以蓝色环突出显示。T2D, 2型糖尿病
结论:IAPP介导的β细胞损伤是2型糖尿病胰岛炎症和去分化的可能机制。抑制IAPP毒性是2型糖尿病潜在的治疗目标。
原文出处:
Blencowe M, Furterer A, Wang Q,et al.IAPP-induced beta cell stress recapitulates the islet transcriptome in type 2 diabetes.Diabetologia 2021 Sep 23
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#BET#
54
#DIA#
60
#转录#
70
#胰岛#
49
#转录组#
56
#应激#
56
好!
75