J Bone Joint Surg Am:转子间骨折螺钉切出的预测因素
2012-08-10 紫川秀第二 丁香园
转子间骨折内固定术后螺钉切出一直是创伤外科治疗的难题,螺钉切出可导致骨折移位和骨折不愈合,影响患者生存质量,往往需要二期手术。目前报道的人为转子间骨折内固定术后螺钉切出的可能预测因素有尖顶距(tip apex distance,TAD,<25mm),骨折类型,螺钉在股骨头内的位置,骨折复位的情况等,但上述预测因子的有效性较少有文章进行评估报道。来自荷兰的学者近期就转子间骨折内固定螺钉切出的有
转子间骨折内固定术后螺钉切出一直是创伤外科治疗的难题,螺钉切出可导致骨折移位和骨折不愈合,影响患者生存质量,往往需要二期手术。目前报道的人为转子间骨折内固定术后螺钉切出的可能预测因素有尖顶距(tip apex distance,TAD,<25mm),骨折类型,螺钉在股骨头内的位置,骨折复位的情况等,但上述预测因子的有效性较少有文章进行评估报道。来自荷兰的学者近期就转子间骨折内固定螺钉切出的有效预测因素进行了专题研究,相关结论近期发表在JBJS am上。
研究共纳入290例转子间骨折的患者,其中214例符合研究的纳入要求,男性47例,女性168例,平均年龄78岁。对纳入研究的患者进行骨折部位的放射学评估,包括骨折的前后位和侧位片。放射学评估的内容包括:骨折的分型(AO标准),骨折复位的质量(良好复位的标准:正位片上颈干角正常或轻度外翻,侧位片上角度<20度,并且侧位片上的骨折断端位移<4mm),螺钉的位置,尖顶距(计算方法如图1)等。
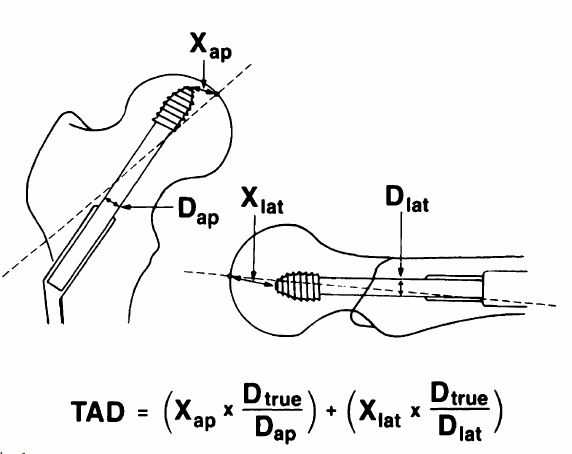
图1:尖顶距计算方法:Dture=螺钉真实直径,Dap=前后位片螺钉的测量直径,Xap=前后位片测量的螺钉距圆弧顶点距离,Dlat=侧位片螺钉的测量直径,Xlat=侧位片测量螺钉距圆弧顶点的距离
研究结果提示:共16例(7.4%)病人发生螺钉切出而出现内固定失败,其中3个病人在术后3个月后螺钉发生切出,而其余13例病人螺钉切出发生在3个月内。此外有6例病人因为其他原因需要二次手术进行骨折内固定。
对相关因素进行分析:
可靠性分析:TAD(tip apex distance),单人或多人组内相关性系数分别为0.81及0.89,提示具有很高的可靠性;而骨折复位和螺钉位置和螺钉切出呈中度可靠性(相关系数分别为0.48及0.46)。
表1:不同观察者变量观察的可靠性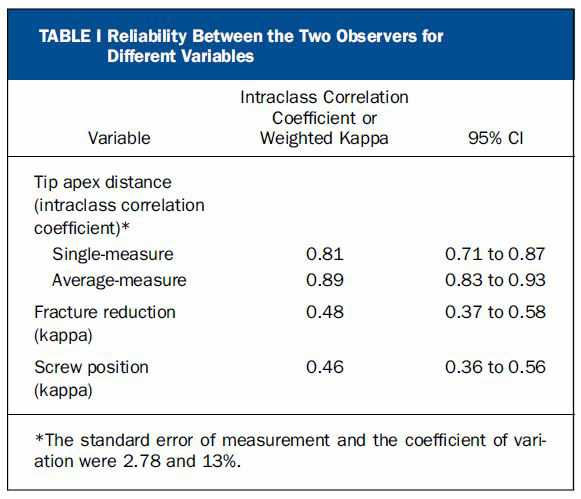
单因素分析:螺钉切出病人的平均TAD为25.9±8.6mm,而未切出病人平均TAD为21.3±6.1mm,组间比较差异较为显著;病人的年龄,性别,手术时间,住院天数,伤后手术开始的时间等组间比较无明显差异;AO分类系统中A3骨折类型的病人与A1 病人比OD值为3.2,但两者间无明显的差异;手术复位较好的病人较手术复位差的病人,切除率较低,两者有显著差异;螺钉置于中下方和前下方时可以有效地防止螺钉切割的发生。表2
表2:螺钉切出和螺钉未切出病人的整体统计数据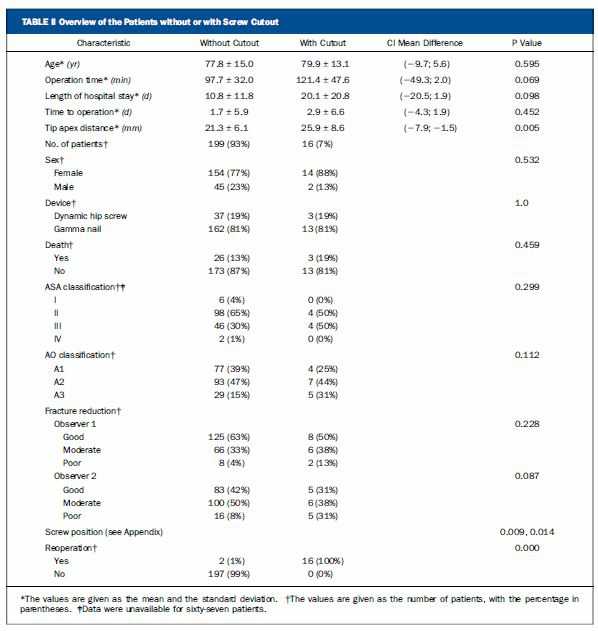
多因素分析:为确定合适的TAD,使用ROC曲线法(图2),结果显示19.9mm为TAD的一个临界值,敏感性87.5%,特异性44.7%;而使用传统的25mm作为临界值时,敏感性50%,特异性71.4%。作者认为,对25mm而言,其做为螺钉不切出的标准值意义更大。
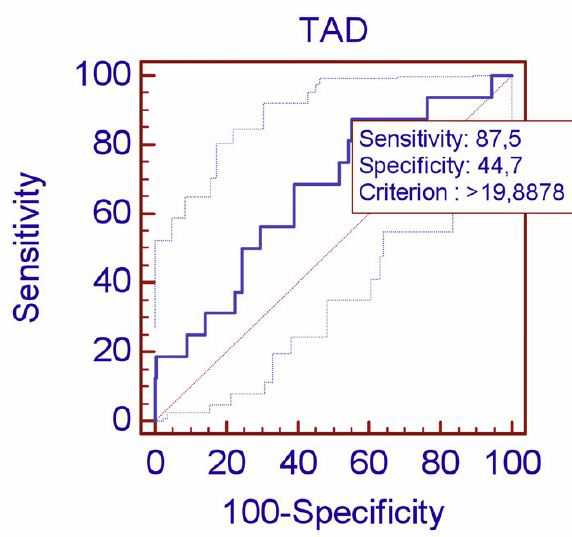
作者最后得出结论:对股骨转子间骨折的患者而言,螺钉置入股骨头时TAD最好小于25mm,20mm是一个较为可靠的指标,并且位置最好在股骨头的中或者前下方,在临床实践中要特别注意A3骨折,这类病人螺钉容易切出。
原文链接: De Bruijn K, den Hartog D, Tuinebreijer W, Roukema G. Reliability of predictors for screw cutout in intertrochanteric hip fractures. J Bone Joint Surg Am. 2012 Jul 18;94(14):1266-72.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言








#Bone#
38
#转子间#
51
#预测因素#
39