Chest:COPD患者的心血管风险
2019-11-22 xing.T MedSci原创
由此可见,对未选择的原因不同的COPD患者分析表明:1)COPD本身不足以解释其增加aPWV,2)吸烟是COPD患者aPWV增加的危险因素。
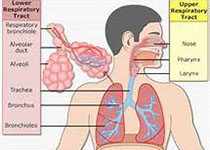
慢性阻塞性肺疾病(COPD)是心血管疾病(CVD)的独立危险因素,这一发现来自对患有COPD的吸烟者和未患有COPD的吸烟者进行比较。尚不清楚COPD患者CVD风险增加的机制。近日,呼吸领域权威杂志chest上发表了一篇研究文章,该研究旨在评估系统性动脉僵硬度(CVD死亡率的预测指标),并评估因有机粉尘暴露、吸烟或两者均有引起的轻度至中度COPD患者的决定因素。
研究人员通过主动脉脉搏波速度(aPWV)评估全身动脉僵硬度。对142名COPD患者和155名健康对照者进行了测量,并匹配了受试者年龄、性别、体重指数和吸烟、暴露于香烟(COPD/对照分别为=56/70)、有机粉尘(n=44/48)或两者兼有(n=42/37)。主
相比暴露于吸烟,烟尘和粉尘均有的健康对照者,COPD患者的PWV更高。相比之下,在接触有机粉尘的不吸烟者中,COPD患者和相匹配的对照者的aPWV相似。对142名COPD患者(暴露于吸烟和/或有机粉尘)的多变量分析表明,吸烟与高aPWV有关。此外,这些患者中主要心血管事件的标志物,可溶性致癌抑制因子2(ST2)与aPWV相关。
由此可见,对未选择的原因不同的COPD患者分析表明:1)COPD本身不足以解释其增加aPWV,2)吸烟是COPD患者aPWV增加的危险因素。
原始出处:
Thibaud Soumagne,et al.Cardiovascular Risk in COPD: Deciphering the Contribution of Tobacco Smoking.chest.2019.https://doi.org/10.1016/j.chest.2019.11.002
本文系williamhill asia
医学(MedSci)原创编译整理,转载需授权!
小提示:本篇威廉亚洲官网
需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#Chest#
68
#EST#
63
#血管风险#
67
好
112
#COPD患者#
74