Cardiovasc Diabetol :预测2型糖尿病合并动脉粥样硬化性心血管疾病患者心血管死亡、非致命性心肌梗死或非致命性中风的模型的建立和验证
2022-09-22 从医路漫漫 MedSci原创
与非糖尿病患者相比,T2DM患者发生主要心血管不良事件(MACE )(定义为心血管(CV)死亡、心肌梗死(MI)和中风)的可能性几乎是非糖尿病患者的三倍。
背景:在患有动脉粥样硬化性心血管疾病(ASCVD)的个体中,二型糖尿病(T2DM)是常见的,并且增加了发病率和死亡率的风险。同样,与非糖尿病患者相比,T2DM患者发生主要心血管不良事件(MACE )(定义为心血管(CV)死亡、心肌梗死(MI)和中风)的可能性几乎是非糖尿病患者的三倍。因此,预防MACE已经成为T2DM患者临床试验、治疗策略和临床实践威廉亚洲博彩公司 的主要焦点。
理想情况下,这些患者的治疗决策是由患者心血管并发症的潜在风险决定的。然而,到目前为止,这种风险预测的模型是缺乏的,那些可用的具有次优的性能并且是过时的。UKPDS风险引擎在预测T2DM患者ASCVD事件风险方面表现出了合理的准确性,但这是在那些无基线心脏病或中风的患者中以及在T2DM诊断时开发的。相比之下,对于预测同时患有T2DM病和ASCVD的个体的心血管风险的关注相对较少。开发了一个更新的UKPDS结果模型来预测中位持续时间超过17年的继发性心肌梗死和卒中事件,但该风险模型是使用模拟研究开发的,未经外部验证,旨在预测近20年长期随访的风险。考虑到ASCVD患者在4年内发生MACE的可能性是一级预防亚组的两倍以上,患者的风险分层对于治疗决策非常重要。
目的:在这项研究中,williamhill asia 的目的是开发一个模型,预测同时患有T2DM和ASCVD的个体在使用西格列汀(TECOS)评估心血管结局的试验中的中期ASCVD事件,并从外部验证ACCORD(控制糖尿病心血管风险行动)试验参与者的研究结果。
方法:使用西他列汀(TECOS)评估心血管结局试验的数据,williamhill asia 使用Cox比例风险模型预测T2DM和ASCVD患者的MACE。试验中收集的所有基线协变量都被考虑包括在内,尽管有些因为大量遗漏或共线性而被立即排除。在25个估算数据集的每一个中使用逐步选择开发了一个完整的模型,并且包括在25个数据集中的20个中选择的候选变量。使用具有最小绝对收缩和选择算子(LASSO)的Cox模型创建了最大10个自由度的简约模型,其中调整的R平方用作选择标准。然后,该模型在ACCORD(控制糖尿病心血管风险行动)试验中具有相似标准的一组参与者中进行外部验证。使用Harrell的C指数和基于4年事件发生率的Greenwood-Nam-D'Agostino统计的模型校准来评估两种模型的区分度。
结果:总的来说,TECOS的14,671名参与者中有1491名(10.2%)和ACCORD验证队列(n = 1404)的130名(9.3%)在3年的中位随访中出现了MACE。最终模型包括9个特征(既往中风、年龄、慢性肾病、既往心肌梗死、性别、心力衰竭、胰岛素使用、心房颤动和微血管并发症)。该模型在内部和外部验证样本中具有中等的区分度(C指数分别为0.65和0.61)。该模型在整个风险范围内校准良好——从最低风险五分位数的4年累积MACE率为6%到最高风险五分位数的26%。
表1使用扩展风险评分中的变量的多变量调整模型输出参数


图1基于预测风险十分位数的简化和扩展风险评分的预测与观察到的主要心血管不良事件(MACE) 4年发生率。MACE是首次非致死性心肌梗死、非致死性中风或心血管死亡的复合
表2使用简约风险评分中的变量的多变量调整模型输出参数
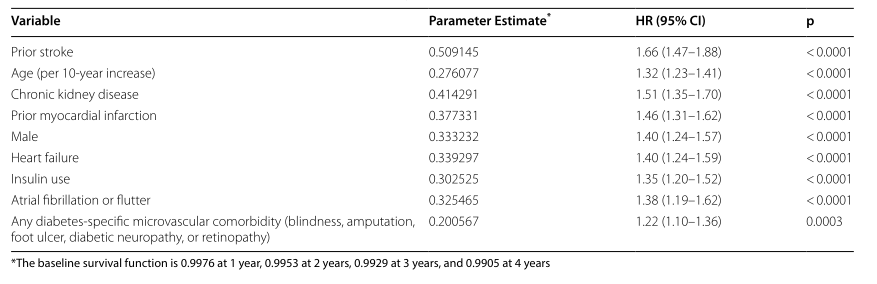
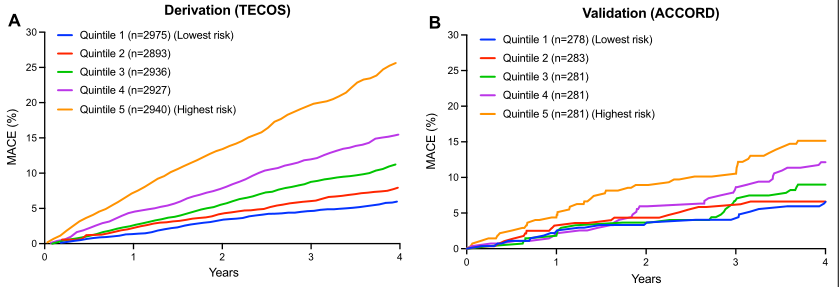
图2 A推导(TECOS)和B验证(ACCORD)队列中风险评分五分位数的MACE累积发生率。MACE是首次非致死性心肌梗死、非致死性中风或心血管死亡的复合
结论:在T2DM和ASCVD患者中,这个9因素风险模型可以量化未来ASCVD并发症的风险,并为治疗和强度决策提供信息。
原文出处: Stevens SR, Segar MW, Pandey A, Development and validation of a model to predict cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke in patients with type 2 diabetes mellitus and established atherosclerotic cardiovascular disease.Cardiovasc Diabetol 2022 Aug 27;21(1)
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言








#疾病患者#
93
#BET#
75
#粥样硬化#
110
#DIA#
115
#ASC#
65
#粥样硬化性#
101
#动脉粥样硬化性心血管疾病#
137
#硬化性#
79
#血管疾病#
110
#心血管死亡#
58