8 招搞定肿瘤患者深静脉血栓形成的抗凝治疗
2016-08-27 子弹头 肿瘤时间
静脉血栓栓塞(VTE)是癌症患者死亡的第二大病因,发生血栓栓塞的癌症患者的总体死亡率高, 1 年生存率只有无栓癌症患者的 1/3。5%~20% 的肿瘤患者会发展为 VTE,放化疗、手术以及转移等因素也可增高血栓风险。VTE 发生的原因可能与肿瘤产生的黏蛋白、组织因子相关因素、半胱氨酸蛋白酶,导致了血栓和局部缺氧相关。1预防性抗凝治疗临床上,考虑是否应用预防性抗凝治疗的因素包括:深静脉血栓史、肿瘤和
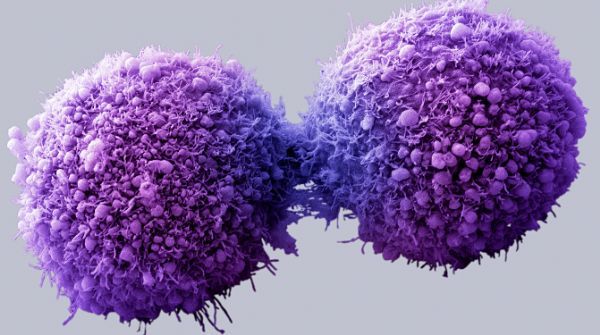
静脉血栓栓塞(VTE)是癌症患者死亡的第二大病因,发生血栓栓塞的癌症患者的总体死亡率高, 1 年生存率只有无栓癌症患者的 1/3。
5%~20% 的肿瘤患者会发展为 VTE,放化疗、手术以及转移等因素也可增高血栓风险。
VTE 发生的原因可能与肿瘤产生的黏蛋白、组织因子相关因素、半胱氨酸蛋白酶,导致了血栓和局部缺氧相关。
1预防性抗凝治疗
临床上,考虑是否应用预防性抗凝治疗的因素包括:深静脉血栓史、肿瘤和腺病引起的血管压迫和遗传性易栓症。
肿瘤患者的血栓风险包括:长期制动、激素治疗、血管生成抑制剂的应用。
门诊接受化疗和预防性抗凝治疗的癌症患者需要密切关注:肾功能、血小板计数,发生改变可能提示有出血风险,应及时停止抗凝治疗。
血小板计数<50000/mm3 ,停止任何剂量的抗凝药物;血栓风险极高的患者,若血小板计数>30000/mm3 ,可以继续预防性抗凝治疗。
ASCO 最新威廉亚洲博彩公司
推荐的抗凝治疗
1. 已确定的深静脉血栓和肺栓塞推荐低分子量肝素用于最初 5~10 天的起始治疗,也可用于至少 6 个月的长期二级预防。
2. 如果没有其他的适应症,抗凝药物不应用作延长癌症患者生存期的治疗。
3. 大多数肿瘤住院患者在整个住院治疗期间须预防血栓。小手术或短期输液化疗患者的常规血栓预防措施没有充分数据支持。
4. 正在行沙利度胺/来那度胺联合化疗或地塞米松治疗的多发性骨髓瘤患者,静脉血栓栓塞发生率为 23%~75%,应以低分子量肝素、低剂量阿司匹林或华法林预防静脉血栓栓塞。
5. 即将接受大型手术的癌症患者,在手术前予预防干预持续至少 7~10 天。接受腹部或盆腔大手术的患者,基于手术的高风险,血栓预防干预时间延长至术后 4 周。
6. 流动的癌症患者不推荐常规血栓预防措施。考虑用于经选择的高风险的患者。
7. 新型口服抗凝血药物目前不推荐。
8. 应对癌症患者定期评估 VTE 风险,对于静脉血栓栓塞风险增高的患者——Khorana 评分 ≥ 3 分或胰腺癌、肺癌、胃癌患者,需向患者介绍预防性抗凝治疗的风险和获益,可预防性剂量的小分子肝素或普通肝素。
2静脉血栓者需要筛查癌症吗?
2015 年 7 月加拿大研究者发表在 NEJM 上一项 854 例患者的研究显示:罹患不明原因静脉血栓的患者隐匿性癌的发病率较低,腹部和骨盆常规 CT 筛查等过多的检查并不能为肿瘤早期诊断提供帮助,反而会使患者受到一些检查所带来的损害。
因此,为了让患者获益更多,临床医师们应该注意「少即是多」。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#静脉血#
46
#静脉#
42
确实不错。
96
很好,不错,以后会多学习
88
#肿瘤患者#
58
#静脉血栓形成#
59
继续学习,感谢分享
81
学习啦,谢谢分享
93