强直性脊柱炎患者颈部增生糜烂恶臭 长期口服青霉素无效后怎么办?
2019-01-14 赵俊英 王增芳 专家会诊中心病例讨论精选
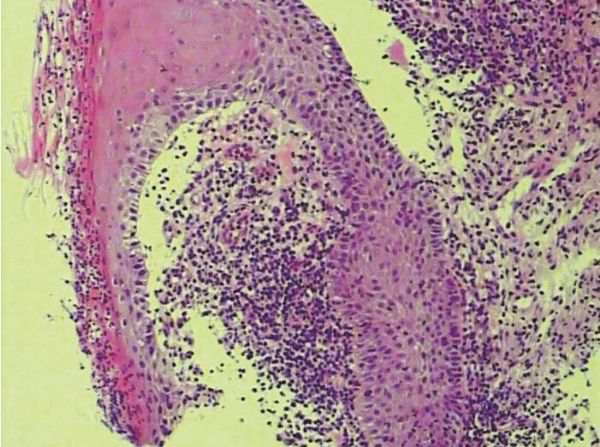
24岁男性,强直性脊柱炎多年,轮椅活动,不能步行。患者2年前右侧颈部出现增生性皮损。口服青霉素类抗生素、外用四环素、红霉素软膏,开始皮损有好转,但反复多次,以后再次口服抗生素等治疗无效。1个月前相同皮损逐渐增多伴有流脓、瘙痒、疼痛,黄色脓性分泌物较多,有恶臭。多家医院就诊,均未得到明确诊断和治疗,原来是真菌感染作祟。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言















#强直性#
55
#脊柱炎#
65
#青霉素#
51
#糜烂#
57
#颈部#
62