季加孚:肿瘤领域如何实现精准医疗的3R理念
2018-01-07 佚名 北京大学医学部
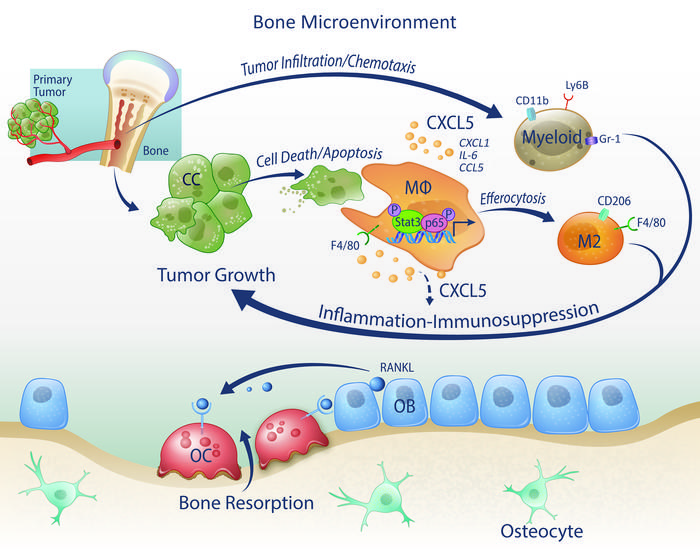
季加孚理解的精准医学,是指根据个体基因特征、环境以及生活习惯进行疾病干预和治疗的最佳方法,涵盖一个大数据,两个体系,三个精准,四个工具。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言











#肿瘤领域#
57
学习了.涨知识
69
不错的文章值得推荐
68
#精准#
55
#季加孚#
71
好好好好好好好好
83
学习学习学习
71
很好的文章.谢谢分享
75