腹膜后肉瘤:伴肠穿孔的2例罕见病例
2011-06-07 MedSci原创 MedSci原创
摘要 腹膜后肉瘤是一种罕见的恶性肿瘤,往往起病隐匿。最常见初始症状包括腹部包块,疼痛或梗阻等。williamhill asia 的这2例患者,表现为腹部不适,诊断为腹膜后肉瘤伴继发性肠穿孔。穿孔是腹膜后肉瘤罕见的一种并发症,但可能会严重影响患者的预后。两名患者均进行了手术切除,且具有恶性肿瘤的病理特征。诊治期间发现肠穿孔应进行经验性抗生素治疗和快速手术治疗
摘要
腹膜后肉瘤是一种罕见的恶性肿瘤,往往起病隐匿。最常见初始症状包括腹部包块,疼痛或梗阻等。williamhill asia 的这2例患者,表现为腹部不适,诊断为腹膜后肉瘤伴继发性肠穿孔。穿孔是腹膜后肉瘤罕见的一种并发症,但可能会严重影响患者的预后。两名患者均进行了手术切除,且具有恶性肿瘤的病理特征。诊治期间发现肠穿孔应进行经验性抗生素治疗和快速手术治疗。
简介
腹膜后肉瘤是一种罕见的无痛性恶性肿瘤。人口估计年发病率为每百万2.7人[1]。典型症状是腹部包块,疼痛,以及一些与相邻腹部脏器受压迫有关的症状 [-8]。文献回顾显示,最常见的发病年龄为五六十岁,无性别差异[1,2,5-9]。 症状常受转移瘤或局部脏器受累影响[4]。这里,williamhill asia 报告2例表现为腹膜后肉瘤的患者,且这2例患者均并发胃肠道穿孔。
病例介绍
患者A是67岁老年女性患者,曾有盆腔平滑肌肉瘤和经腹全子宫切除及双侧输卵管卵巢切除病史,患者出现腹部不适,早饱,体重减轻症状。体检发现一个巨大的,固定的腹部包块。入院实验室检查显示白细胞明显增多(WBC = 45 700)和大肠杆菌血培养阳性。腹部和骨盆CT提示骨盆占位性肿块,腹大部可见气囊性改变,门静脉可疑积气,左肾轻度积水(图1)。
腹膜后肉瘤是一种罕见的恶性肿瘤,往往起病隐匿。最常见初始症状包括腹部包块,疼痛或梗阻等。williamhill asia 的这2例患者,表现为腹部不适,诊断为腹膜后肉瘤伴继发性肠穿孔。穿孔是腹膜后肉瘤罕见的一种并发症,但可能会严重影响患者的预后。两名患者均进行了手术切除,且具有恶性肿瘤的病理特征。诊治期间发现肠穿孔应进行经验性抗生素治疗和快速手术治疗。
简介
腹膜后肉瘤是一种罕见的无痛性恶性肿瘤。人口估计年发病率为每百万2.7人[1]。典型症状是腹部包块,疼痛,以及一些与相邻腹部脏器受压迫有关的症状 [-8]。文献回顾显示,最常见的发病年龄为五六十岁,无性别差异[1,2,5-9]。 症状常受转移瘤或局部脏器受累影响[4]。这里,williamhill asia 报告2例表现为腹膜后肉瘤的患者,且这2例患者均并发胃肠道穿孔。
病例介绍
患者A是67岁老年女性患者,曾有盆腔平滑肌肉瘤和经腹全子宫切除及双侧输卵管卵巢切除病史,患者出现腹部不适,早饱,体重减轻症状。体检发现一个巨大的,固定的腹部包块。入院实验室检查显示白细胞明显增多(WBC = 45 700)和大肠杆菌血培养阳性。腹部和骨盆CT提示骨盆占位性肿块,腹大部可见气囊性改变,门静脉可疑积气,左肾轻度积水(图1)。
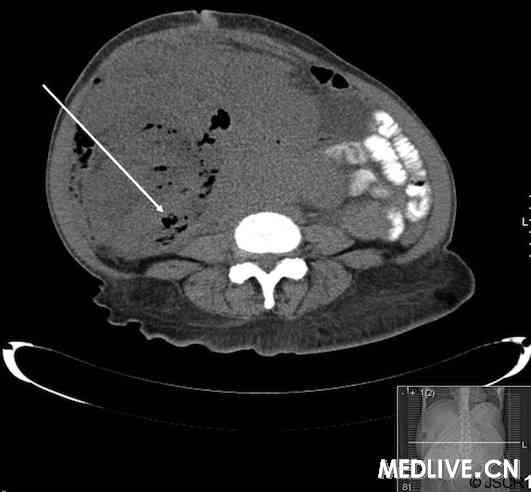
图1:患者A腹部和盆腔CT显示气囊性肿块(箭头所示)。
该患者接受抗生素治疗,并行40厘米腹膜后和盆腔肉瘤切除术。手术期间,发现右半结肠穿孔至肿瘤,可见大量肠液。手术扩大到右半结肠切除,乙状结肠切除及结肠造口术,和节段性小肠切除。病理分析提示为恶性梭形细胞瘤,CD117和CD10免疫组化染色阴性,结蛋白和肌特殊肌动蛋白轻度反应,低度恶性平滑肌肉瘤是最可能的诊断。
三个月随访时,患者A继续康复,未检出癌细胞。考虑到患者肿瘤病理分级为低度恶性,没有必要进行诸如化疗或放疗等辅助治疗。
患者B是61岁老年男性,症状表现为腹痛和体重减轻。体格检查发现左下腹可触及一肿块。尽管患者最初不发热且无感染症状,但检查结果显示患者白包细胞增多(WBC= 76 800)。腹部和盆腔CT检查显示肿块起于左肾,附着在乙状结肠。 CT导引穿刺活检证实为一高级别多形性恶性肉瘤,与恶性纤维组织细胞瘤相一致。进一步的MRI评估证实左腹膜后有一巨大的坏死性肿块,降结肠被气液包裹,考虑为结肠穿孔(图2)。患者开始抗生素治疗并行手术切除。

图2:患者B腹部MRI检查显示降结肠被肿块包裹,且出现气液平面(箭头所示)。
术中,发现腹腔后腔内有游离气体和少量粪便污染。完成左半结肠,腹膜后肉瘤,左肾和肾上腺整块切除(en bloc resection),及结肠造口。病理诊断显示波形蛋白强表达,但无细胞角蛋白CAM5.2,CD15,CD30,CD117,结蛋白和S100蛋白染色的证据,这证实了未分化高级别多形性肉瘤的活检结果。
讨论
肠穿孔是腹膜后肉瘤的一个罕见并发症。文献回顾[2-9]没有发现任何有关腹膜后肉瘤继发肠穿孔的报告。许多病例研究是在普及应用CT和MRI检测腹部疾病之前进行的,这可能限制了识别肠穿孔的能力,同时也对先前研究缺乏相关描述做出了解释。不过,手术预后和并发症的系列研究报道中都没有提到过术中肠穿孔现象,这说明肠穿孔是相对少见的。
由于患者A先前有平滑肌肉瘤病史,并且当前病理检查显示为低度恶性平滑肌肉瘤,williamhill asia 认为这次很可能是先前恶性肿瘤的复发。大量腹膜后肉瘤病例系列研究结果发现平滑肌肉瘤是继脂肪肉瘤之后,第二种最常见的腹膜后肉瘤形式[2]。此病的复发最有可能说明恶性肿瘤发生了慢性生长,但是这一生长过程直到临床病程后期才会引起临床重视。同样,恶性肿瘤长期压迫胃肠道也很可能导致结肠穿孔。由于没有先前病史,患者B的肉瘤可能是一个原发性恶性肿瘤。较之平滑肌肉瘤,恶性纤维组织细胞瘤是一种比较罕见的肉瘤亚型[2]。但是这种肉瘤更具侵袭性,可能促使穿孔继发于肿瘤局部快速生长后发生。
值得注意的是,这2例患者均表现白细胞明显增多。患者A就诊时血培养阳性表明存在传染性病因,最有可能继发于肠穿孔,这可能是其白细胞增多的原因。患者B就诊时血培养阴性,其白细胞增多更有可能是一种类白血病反应。
手术切除仍是腹膜后肉瘤治疗的主要方法[1],患者手术切除率为54-88%不等[10]。尽管做了这些努力,但局部复发仍较常见。预后与手术切缘的明确程度以及肉瘤的分化等级有很大关系[2]。患者B恶性肿瘤的快速复发和预后较差可能与其肉瘤的高度恶性以及未分化特点有关。病人A未检出其他疾病(癌症),将继续接受每6个月一次的CT复发检查和随访。
胃肠穿孔是腹膜后肉瘤的一种罕见的、具有临床意义的潜在并发症。临床诊断中发现该病症应给予及时的抗生素初始治疗和行外科干预。
参考文献
[1] Porter GA, Baxter NN, Pisters PW: Retroperitoneal sarcoma: a population-based analysis of epidemiology, surgery, and radiotherapy. Cancer 2006, 106(7):1610-1616
[2] Lewis JJ, Leung D, Woodruff JM, Brennan MF: Retroperitoneal soft-tissue sarcoma: analysis of 500 patients treated and followed at a single institution. Ann Surg 1998, 228(3):355-365
[3] Pirayesh A, Chee Y, Helliwell TR, Hershman MJ, Leinster SJ, Fordham MV, Poston GJ: The management of retroperitoneal soft tissue sarcoma: a single institution experience with a review of the literature. Eur J Surg Oncol 2001, 27(5):491-497
[4] Cheifetz R, Catton CN, Kandel R, O’Sullivan B, Couture J, Swallow CJ: Recent progress in the management of retroperitoneal sarcoma. Sarcoma 2001, 5(1):17-26
[5] Wist E, Solheim OP, Jacobsen AB, Blom P: Primary retroperitoneal sarcomas. A review of 36 cases. Acta Radiol Oncol 1985, 24(4):305-310/a>
[6] Salvadori B, Cusumano F, Delledonne V, De Lellis R, Conti R: Surgical treatment of 43 retroperitoneal sarcomas. Eur J Surg Oncol 1986, 12(1):29-33
[7] Zornig C, Weh HJ, Krull A, Schwarz R, Hilgert RE, Schroder S: Soft tissue sarcomas of the extremities and trunk in the adult. Report of 124 cases. Langenbecks Arch Chir 1992, 377(1):28-33
[8] Alvarenga JC, Ball AB, Fisher C, Fryatt I, Jones L, Thomas JM: Limitations of surgery in the treatment of retroperitoneal sarcoma. Br J Surg 1991, 78(8):912-916
[9] Singer S, Corson JM, Demetri GD, Healey EA, Marcus K, Eberlein TJ: Prognostic factors predictive of survival for truncal and retroperitoneal soft-tissue sarcoma. Ann Surg 1995, 221(2):185-195
[10] Hueman MT, Herman JM, Ahuja N: Management of retroperitoneal sarcomas. Surg Clin North Am 2008, 88(3):583-597
原文链接
Retroperitoneal sarcoma: a rare cause of intestinal perforation in two cases
小提示:本篇威廉亚洲官网
需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言








#腹膜后#
72
#罕见病例#
84
#腹膜后肉瘤#
63
专注啊
180
#穿孔#
71
#罕见#
67
#肠穿孔#
61
#腹膜#
67