Lancet Oncol:纳武单抗联合卡博替尼治疗晚期肾细胞癌的长期预后
2022-06-12 MedSci原创 MedSci原创
纳武单抗联合卡博替尼治疗晚期肾细胞癌的效果明显优于舒尼替尼!
在CheckMate 9ER试验的主要分析(中位随访了18.1个月)中,与舒尼替尼相比,纳武单抗联合卡博替尼在既往未治疗过的晚期肾细胞癌患者的无进展生存期、总生存期和客观缓解率方面展现出了显著的优越性。本文报告了该试验延长随访的总生存期和最新的疗效和安全性分析结果。
CheckMate 9ER是一项在18个国家的125家医院/癌症中心开展的开放标签的随机化3期试验,招募了年满18睡的既往未治疗过的晚期或转移性肾透明细胞癌患者,且要求Karnofsky表现状态≥70%。患者被(1:1)随机分至纳武单抗+卡博替尼组或舒尼替尼组。主要终点是无进展生存期。次要终点是总生存期。
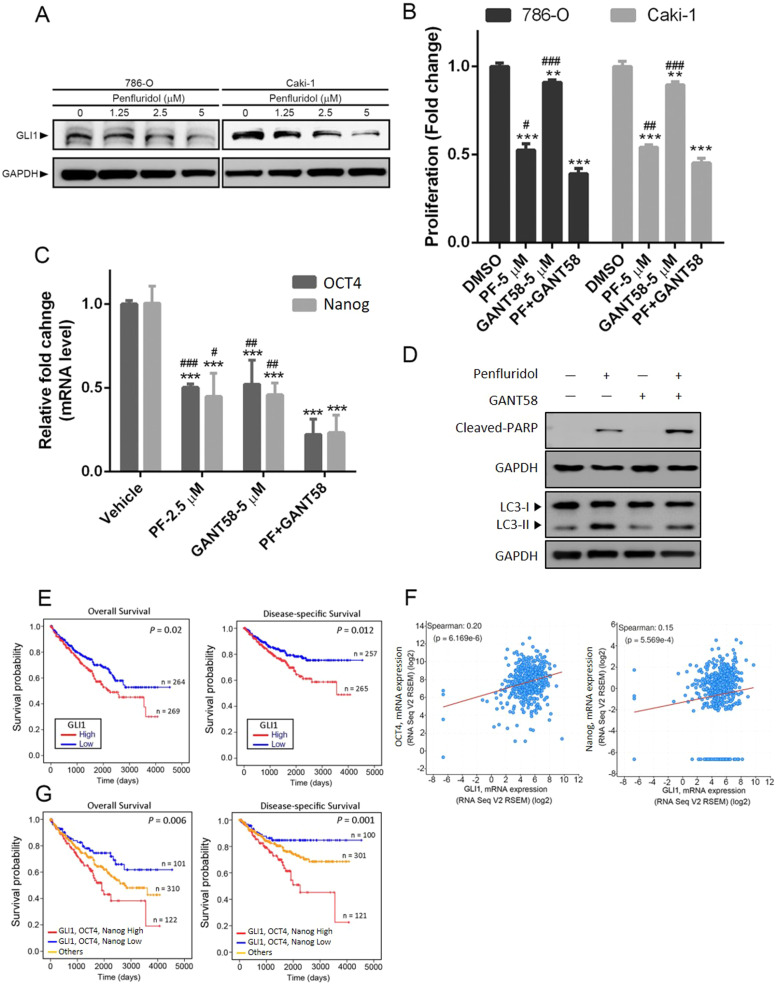
两组患者的总生存率(A)和无进展生存率(B)
2017年9月11日至2019年5月14日,共651位患者被随机分至联合组(n=323)或舒尼替尼组(n=328)。截止2021年6月24日,中位随访了32.9个月,联合组和舒尼替尼组的中位总生存期分别是37.7个月和34.3个月(风险比[HR] 0.70,p=0.0043),两组最新的中位无进展生存期分别是16.6个月和8.3个月(HR 0.56,p<0.0001)。
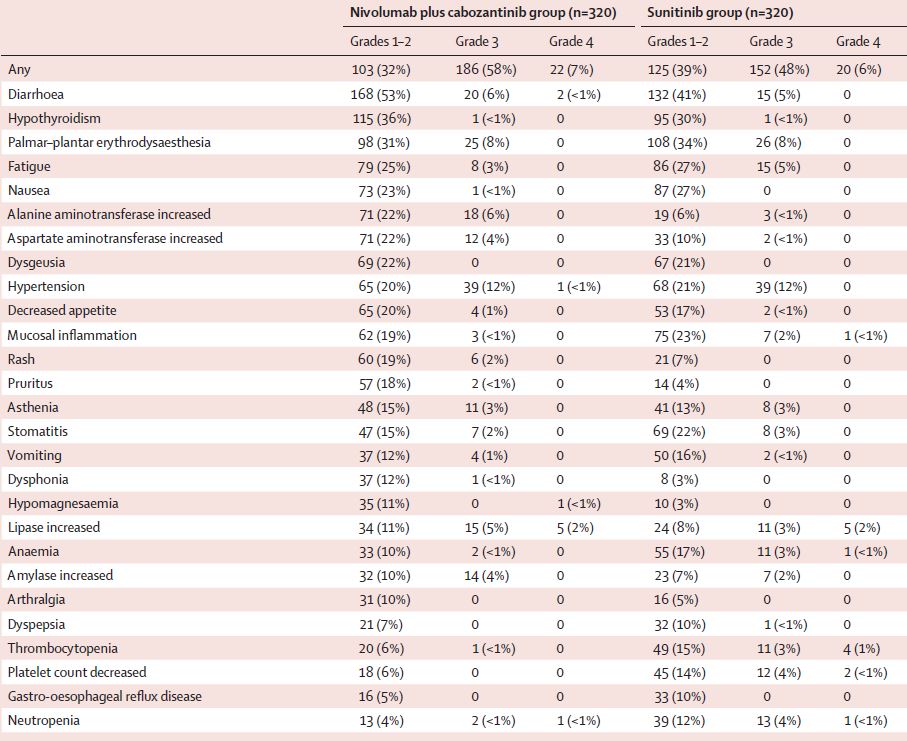
两组治疗相关的不良反应
联合组有208位(65%)患者发生了3-4级的治疗相关的不良事件,舒尼替尼组有172位(54%)。最常见的3-4级治疗相关不良事件有高血压(联合组 vs 舒尼替尼组:13% vs 12%)、掌跖红斑感觉(8% vs 8%)和腹泻(7% vs 5%)。联合组和舒尼替尼组分别有70位(22%)和31位(10%)患者经历了3-4级治疗相关的严重不良反应。舒尼替尼组新发生了一例治疗相关死亡(猝死)。
总而言之,在CheckMate 9ER试验的延长随访过程中,与舒尼替尼相比,纳武单抗联合卡博替尼显示出了更好的疗效,进一步支持该联合方案用作晚期肾细胞癌的一线治疗方案。
原始出处:
Robert J Motzer, et al. Nivolumab plus cabozantinib versus sunitinib in first-line treatment for advanced renal cell carcinoma (CheckMate 9ER): long-term follow-up results from an open-label, randomised, phase 3 trial. The Lancet Oncology. June 07, 2022. https://doi.org/10.1016/S1470-2045(22)00290-X
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#长期预后#
60
#Lancet#
50
#细胞癌#
47
#Oncol#
64
学习学习
61
好好学习
56
#晚期肾细胞癌#
54
lancet上果然牛,感谢williamhill asia 更新及时
52