JACC:经导管主动脉瓣置换术后发生ST段抬高型心肌梗死的患者的临床特征及预后
2021-05-02 MedSci原创 MedSci原创
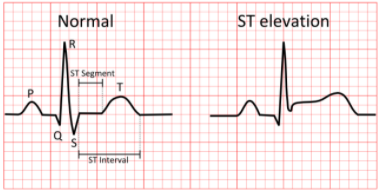
经导管主动脉瓣置换术(TAVR)后发生急性冠脉综合征的患者发生ST段抬高型心肌梗死(STEMI)的风险最高
经导管主动脉瓣置换术(TAVR)后发生急性冠脉综合征的患者发生ST段抬高型心肌梗死(STEMI)的风险最高。
本研究目的是确定TAVR术后发生STEMI的患者的临床特征、治疗和预后。
这是一项多中心研究,纳入了118名在TAVR后中位255天(四分位数范围:9-680天)时出现STEMI的患者。此外,研究人员还将原发性经皮冠状动脉介入治疗(PCI)进行TAVR治疗后的STEMI程序特征与所有STEMI进行了比较:439例非TAVR患者。
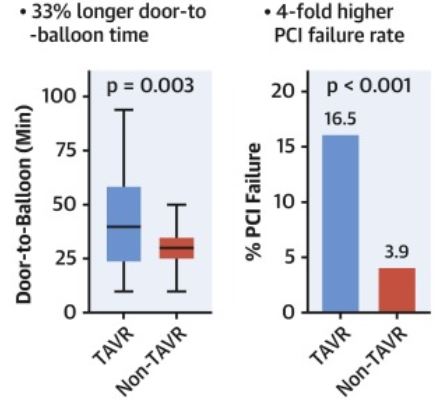
TAVR和非TAVR患者的door-to-balloon时间与PCI失败率
TAVR患者从入门到球囊(door-to-balloon)的中位时间较长(40分钟[四分位数范围:25~57] vs 30分钟[25~35];p=0.003)。TAVR患者的手术时间、透视时间、剂量面积乘积和对比度也较高(均p<0.01)。有TAVR史的患者PCI的失败率较高(16.5% vs 3.9%;p<0.001),其中5例患者因冠脉插管失败而未对病变进行血运重建。
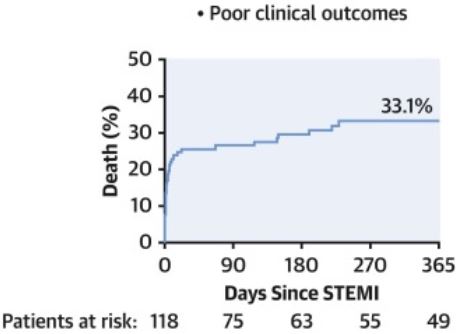
TAVR术后STEMI患者的死亡率
TAVR术后STEMI患者的院内和晚期(中位7个月[四分位数范围:1~21个月])死亡率分别为25.4%和42.4%(直接经皮冠状动脉介入治疗患者的分别为20.6%和38.2%)。估计肾小球滤过率<60 ml/min(危险比[HR] 3.02;95%CI 1.42~6.43;P=0.004)、Killip分级≥2(HR 2.74;95%CI 1.37~5.49;p=0.004)、冠状动脉介入治疗失败(HR 3.23;95%CI 1.42%~7.31%;p=0.005)均可增加死亡风险。
总而言之,TAVR后STEMI与非常高的住院和中期死亡率相关。在TAVR患者中观察到更长的door-to-balloon时间和更高的PCI失败率,部分原因是TAVR人群特有的冠状动脉接入问题,这与预后较差相关。
原始出处:
Faroux Laurent,Lhermusier Thibault,Vincent Flavien et al. ST-Segment Elevation Myocardial Infarction Following Transcatheter Aortic Valve Replacement. J Am Coll Cardiol, 2021, 77: 2187-2199.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#JACC#
49
#临床特征#
43
#置换#
61
#主动脉瓣置换术#
50
#ST段#
78
#置换术#
53
#经导管主动脉瓣置换#
66
#经导管#
64
#ST段抬高#
84
#主动脉#
52