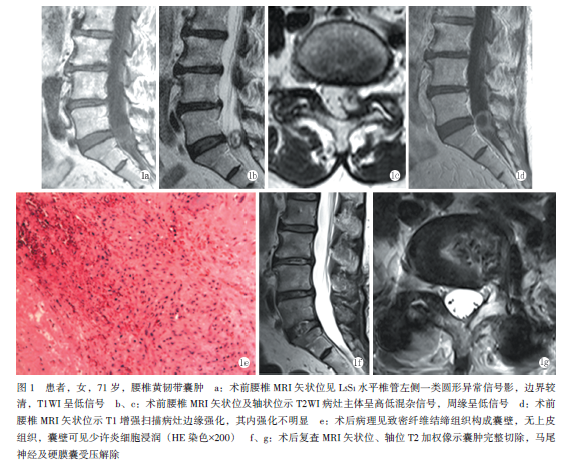
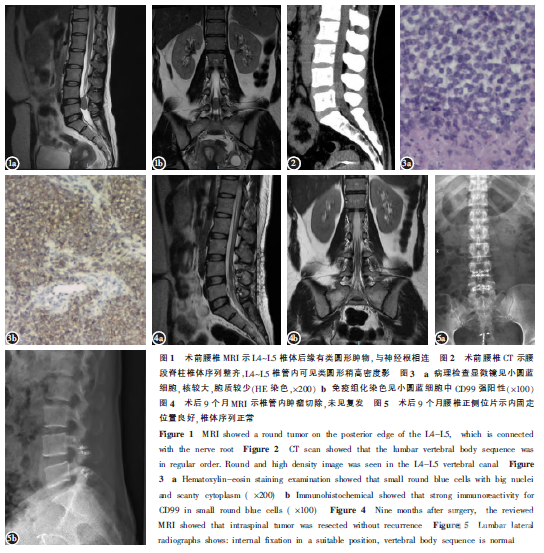
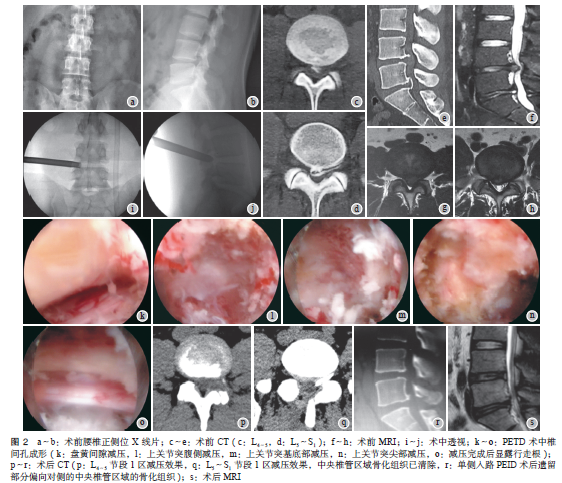
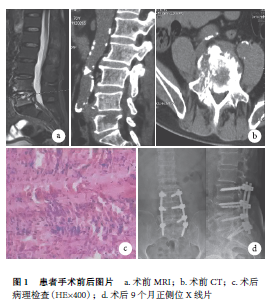
腰椎黄韧带囊肿1例
2019-07-11 袁凯 温广伟 许岳荣 中国矫形外科杂志
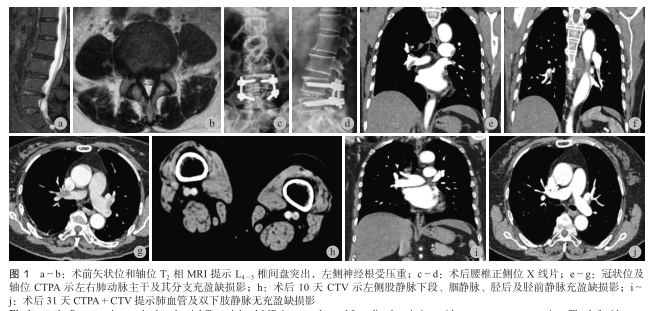
患者,女性,71岁,主诉因“腰痛伴左下肢麻痛6个月余”入院。6个月前患者无明显诱因出现间断性腰部疼痛,伴左下肢麻痛感,以小腿后外侧、足底为主,腰部活动轻微受限。劳累后加重,休息后症状缓解不明显,白天、夜间疼痛无差别,保守治疗后缓解不明显。查体:双下肢肌力5级,左下肢腱反射正常引出,左下肢S1皮节支配区浅感觉减退,左下肢直腿抬高试验阳性(40°),括约肌功能正常。腰椎MRI:L5S1水平椎管左侧见一
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言









#黄韧带囊肿#
58
#黄韧带#
65
#腰椎#
49
#囊肿#
40
#韧带#
43