Blood:CD19-CAR-T细胞的内源性TCR表达的去留?
2020-06-07 QQY MedSci原创
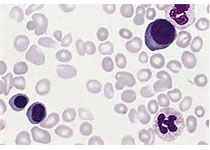
抗CD19-CAR表达的CRISPR/Cas9介导的T细胞受体敲除使allo-CAR-T细胞治疗成为可能;内源性TCR和CD19-CAR的共表达延长了T细胞的体内持久性。
在本研究中,研究人员在原代T细胞中,结合含有4-1BB共刺激结构域的二代逆转录病毒CAR转导,用CRISPR/Cas9介导敲除了TCRb链。
经上述处理,研究人员得到了高功能的TCR-KO-CAR-T细胞群,这些细胞具有强烈的活化(CD25、IFN-小鼠血清)、增殖和对CD19靶点识别的特异性杀伤。TCR-KO-CAR-T细胞具有中心记忆和效应记忆T细胞的平衡表型。与表达TCR的T细胞相比,敲除T细胞内源性TCR强烈地减弱了异体反应性。在一个ALL患儿的异种移植物模型中,TCR-KO-CAR-T细胞明确地控制了CD19+白血病负担,提高了移植小细胞的体内存活率。
但内源性TCR和CAR的共表达可使T细胞获得优异的持久性,并显著延长了白血病的体内控制时间,这一点在第二个使用NALM6白血病细胞的体内模型中得到了证实。上述结果提示内源性TCR对反应寿命具有重要作用。
总而言之,用CRISPR/Cas9介导的TCR KO的抗CD19 CAR T细胞是非匹配的第三方过继T细胞移植的极具潜力的选择,在无异体反应的情况下具有很高的抗白血病功能,但有内源性TCR表达时的体内反应持久性更好。
原始出处:
Dana Stenger,et al. Endogenous TCR promotes in vivo persistence of CD19-CAR-T cells compared to a CRISPR/Cas9-mediated TCR knockout CAR. Blood. June 1,2020.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#CAR-#
67
#内源性#
84
#CD19#
69
#TCR#
71