Stroke:冠状动脉粥样硬化与脑白质高信号之间的关联
2021-05-20 MedSci原创 MedSci原创
在健康的高风险个体中,冠状动脉斑块的存在和体积与更大的WMH体积相关,对于PVWMH而言关联性最强。在高危家庭中的这些结果表明,除了传统的危险因素之外,可能是由于遗传易感性,介导了这两种不同血管床的疾
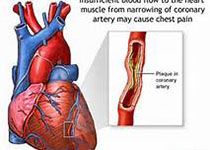
近日,心血管疾病领域权威杂志Stroke上发表了一篇研究文章,研究人员旨在明确健康的高危成年人亚临床冠状动脉疾病与白质高信号(WMH)的数量和位置之间的关联,且与动脉粥样硬化的危险因素无关。

研究人员分析了来自动脉粥样硬化风险遗传学研究(GeneSTAR)研究早发型冠心病(<60岁)病例的782例无症状一级亲属,他们同时接受了冠状动脉计算机断层扫描血管造影和脑磁共振成像检查。

考虑到家庭结构,研究人员采用多级混合效应线性回归模型评估了总的WMH体积和3个区域(深部WMH、室周WMH [PVWMH]或边界带[cuff])与冠状动脉疾病标记之间的关联。研究人员为总WMH、深部WMH、PVWMH和cuff体积创建了单独的模型,并针对协变量进行了调整。

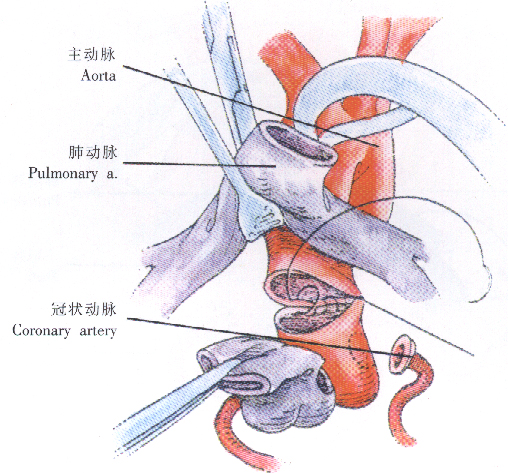
冠状动脉粥样硬化与脑白质高信号
受试者平均年龄为51±10岁,其中58%为女性,39%为非裔美国人。伴有冠状动脉斑块的参与者WMH量比无斑块的参与者大52%(95%CI为0.24-0.59)。冠状动脉斑块体积每增加1%,WMH总量就增加0.07%(95%CI为0.04-0.10)。当与深部WMH与PVWMH(相互作用P<0.001)或cuff体积(相互作用P<0.001)比较时,总冠状动脉斑块体积每增加1%,则深部WMH体积增大(5.0%)(95%CI为4.67–5.38),PVWMH体积增大5.10%(95%CI为4.72–5.48)和cuff体积增大2.74%(95%CI为2.38–3.09)。
由此可见,在健康的高风险个体中,冠状动脉斑块的存在和体积与更大的WMH体积相关,对于PVWMH而言关联性最强。在高危家庭中的这些结果表明,除了传统的危险因素之外,可能是由于遗传易感性,介导了这两种不同血管床的疾病关系。
原始出处:
Michelle C. Johansen.et al.Association of Coronary Artery Atherosclerosis With Brain White Matter Hyperintensity.stroke.2021.https://www.ahajournals.org/doi/10.1161/STROKEAHA.120.032674
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言









#冠状动脉粥样硬化#与#脑白质#
95
#白质#
54
#粥样硬化#
52
#高信号#
83
#白质高信号#
60
#脑白质高信号#
50