2022 ASCO:转移性肝内胆管癌合并肝外疾病患者的局部放射治疗可保护肝功能
2022-06-01 紫菀款冬 MedSci原创
局部肝定向放射疗法(RT)治疗转移性肝内胆管癌(mICC)患者的肝功能保护。
背景:肿瘤相关肝功能衰竭(TRLF)是转移性肝内胆管癌(mICC)患者最常见的死亡原因,在仅接受全身治疗的患者中死亡率高达72%。该研究介绍了用局部肝定向放射疗法(RT)治疗mICC患者的经验。
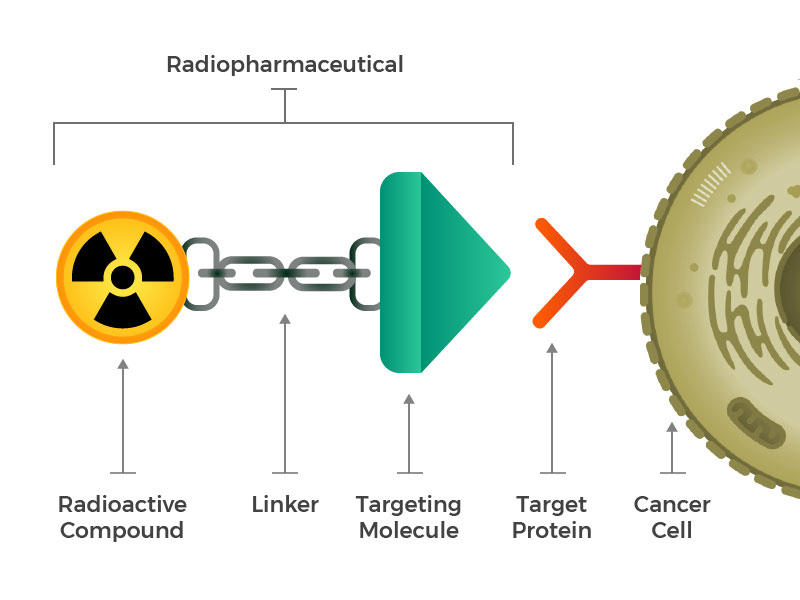
方法:该研究纳入了2011年1月1日至2021年3月31日期间在某中心接受生物等效剂量(BED)至少为50 Gy的放射治疗的肝外转移性疾病ICC患者。记录患者、肿瘤和治疗特征以及生存结果。如果患者死于肝功能衰竭,则认为TRLF为死因;计算RT后1年和2年的TRLF自由度(FFTRLF)。
结果:67名患者被纳入研究。中位年龄为63岁(范围29-83岁),中位放疗剂量为60 Gy(范围,40-100 Gy)。73.1%的患者接受了BED > 80.5 Gy。除1名患者外,所有患者均接受了前期诱导化疗,随后对肝脏原发灶进行放疗,同时(71.6%)或不接受(28.4%)同步化疗。最常用的诱导化疗方案是吉西他滨和顺铂(65.7%),其次是吉西他滨、顺铂和紫杉醇(22.4%),而最常见的同步全身治疗是卡培他滨。
在43名卫星病患者中,29名接受了主要肝脏病变的放疗,而14名接受了原发灶以及一个或多个卫星的放疗。总体而言,15名患者(22.4%)有放射病灶局部进展,42名患者(62.7%)在肝脏其他部位进展,52名患者(77.6%)有远处进展。TRLF是28.4%患者的死因。诊断后的中位OS为25个月,而RT后的中位OS为11.9个月。FFTRLF 1年和2年发生率分别为73.1%和58.2%,显著高于RT后1年和2年OS(分别为47.1%和24.7%,p < 0.005)。
单变量分析未发现 FFTRLF 或 OS 与年龄、性别、体能状态、肝脏病变大小、T或N分期、卫星变、血管血栓形成、TRLF、转移时间、转移部位、RT技术和剂量以及化疗之间存在显著关联。
结论:与历史数据相比,肝外疾病mICC患者的肝脏定向放射治疗似乎具有良好的TRLF率和生存时间。未来的前瞻性研究有必要确定这些患者因放射治疗而带来的生存获益。+
原始出处:
Rituraj Upadhyay, et al. Preservation of liver function with local radiation therapy in patients with metastatic intrahepatic cholangiocarcinoma with extrahepatic disease.
https://meetings.asco.org/abstracts-presentations/211212
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言











#疾病患者#
59
#ASC#
58
#肝内胆管癌#
77
#肝功能#
52
#转移性#
63
#局部#
55
#胆管#
72