Cell Rep:什么物质能阻止神经细胞退化?
2019-05-28 佚名 生物通
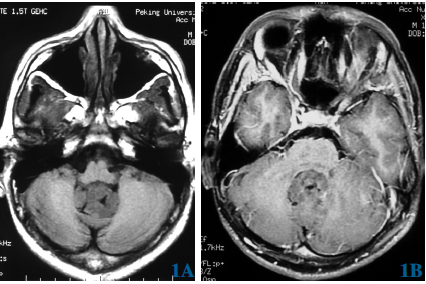
杜克-新加坡国立大学医学院(Duke-NUS Medical School)的一项研究发现,以在基因调控中的作用而闻名的多蛋白“整合子复合体(Integrator complex)”成员,对于果蝇的大脑健康发育至关重要。这一发现对进一步理解和治疗人类神经发育障碍具有指导意义。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#CEL#
46
#Cell#
45
#神经细胞#
61
学习中
0