JACC:氯沙坦作为马凡综合征长期治疗药物安全有效
2018-10-01 MedSci MedSci原创
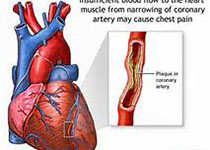
β受体阻滞剂是马凡综合征(MFS)患者的标准疗法,但有研究表明氯沙坦对MFS的有效性存在争议。本研究的目的旨在比较和评估氯沙坦与阿替洛尔在预防MFS主动脉扩张和其他并发症中的有效性。本研究纳入了128例LOAT临床研究中的患者,其中64例接受阿替洛尔治疗,64例接受氯沙坦治疗。经过平均6.7 ± 1.5年时间的随访,共9例不良事件(14.1%)发生在氯沙坦组,12例(18.8%)发生在阿替洛尔组。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#氯沙坦#
86
#治疗药物#
57
#长期治疗#
67
#JACC#
52
#ACC#
64
#综合征#
42
学习了
103