盘点:机械通气有了,那么无创通气优势更大吗?
2016-10-25 MedSci MedSci原创
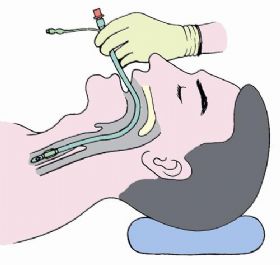
无创通气可以避免气管插管和气管切开引起的很多并发症,近年来得到了广泛的推广和应用。尽管很多随机对照试验证实无创通气治疗慢性阻塞性肺疾病和心源性肺水肿导致的急性呼吸衰竭的疗效肯定,但是无创通气在急性低氧性呼吸衰竭(AHRF)中的应用却存在很多争议。迄今为止,仅有少量的研究表明无创通气可以降低急性肺损伤患者气管再插管率,尚无足够的资料显示无创通气可以作为 ARDS 导致的低氧性呼吸衰竭的常规治疗方
无创通气可以避免气管插管和气管切开引起的很多并发症,近年来得到了广泛的推广和应用。尽管很多随机对照试验证实无创通气治疗慢性阻塞性肺疾病和心源性肺水肿导致的急性呼吸衰竭的疗效肯定,但是无创通气在急性低氧性呼吸衰竭(AHRF)中的应用却存在很多争议。迄今为止,仅有少量的研究表明无创通气可以降低急性肺损伤患者气管再插管率,尚无足够的资料显示无创通气可以作为 ARDS 导致的低氧性呼吸衰竭的常规治疗方法。这里williamhill asia
小编整理了近期关于无创通气的研究与大家共同学习。
【1】无创通气会增加老年肺炎患者的死亡率吗?
本研究的目的是确定现实世界中,机械通气和肺炎患者结局间的关系。研究人员对医疗保险受益人(年龄>64岁)进行了一项回顾性队列研究。干预是无创通气与有创机械通气。
65747例需要机械通气的肺炎患者(医疗保险受益人)中,12480(19%)例接受无创通气。接受无创通气的患者更有可能年龄大、男性、白人、居住在农村、合并症更少、不太可能是器官衰竭类的急性疾病。工具变量分析显示,对于边际患者,接受无创通气与有创机械通气相比,与30天死亡率无关,但是与更低的医保支出有关。
结果表明,接受机械通气的肺炎患者,无创通气与30天死亡率无关。不过还需要进一步的研究来验证和重复这些结果。(文章详见——Crit Care Med:无创通气会增加老年肺炎患者的死亡率吗?)

【2】无创通气改善不伴有OSA肥胖低通气综合征患者呼吸功能
近日,呼吸疾病领域权威杂志《Thorax》发表了一篇西班牙学者进行的多中心随机对照临床研究的文章,该项目旨在确定NIV对不伴有严重OSA的OHS患者的治疗效能。
研究者纳入了从2009年5月至2014年12月期间依次筛选的没有严重的OSA的OHS患者,根据干预因素的不同,参与者被随机分为NIV与改良生活方式两组,随访2个月 。参与者白天动脉二氧化碳分压(PaCO2)作为主要的测量指标,同时研究者对参与者的动脉血气指标、临床症状、与健康相关的生活质量评估、多导睡眠图、肺功能、6分钟步行距离、血压和医疗资源的利用率进行评价,使用意向性治疗分析进行统计分析。
研究共筛选出365例患者,其中58例被排除在外。221例患者有严重的OSA,其余86例患者不伴有严重的OSA。相比于改善生活方式组,NIV组PaCO2和血清碳酸氢盐水平显著升高。调整NIV治疗的依从性,PaCO2的变化并不能进一步提高组间的统计学意义。与改变生活方式组比,NIV治疗组患者嗜睡、与健康相关的生活质量评估和多导睡眠图参数也可显著改善,此外,还有降低NIV组医疗资源利用的趋势。
由此可见,NIV比改善生活方式更能有效的改善日间PaCO2、嗜睡和睡眠指标。此外,需要长期的前瞻性研究来确定NIV是否能够减少医疗资源的利用、心血管事件和死亡率。(文章详见——Thorax: 无创通气改善不伴有OSA肥胖低通气综合征患者呼吸功能)
【3】头盔式无创通气可显著降低ARDS患者的气管插管率
对于急性呼吸窘迫综合症(ARDS)患者来说,经面罩无创通气(NIV)并不能有效预防气管内插管。而经头盔式NIV或是更好的一种治疗方式。本研究旨在确定经头盔NIV能否降低ARDS患者的气管插管率。
采用中心随机临床试验设计,共纳入了2012年10月3日至2015年9月21日在芝加哥大学内科ICU需要接受经面罩进行NIV至少8小时的83名ARDS患者(45%为女性;中位年龄为59岁;中位APACHE II评分为26)。
将这些患者随机分为继续接受面罩NIV治疗组和经头盔进行NIV治疗组,预计招募206名患者(每组各103名)。研究所采用的头盔为一个覆盖患者整个头部的透明罩,在颈部还有一个橡胶密封圈。最后头盔NIV组纳入44名患者,面罩治疗组纳入39名患者,试验提前终止。
结果发现,面罩NIV组插管率为61.5% (n = 24),头盔NIV组插管率为18.2% (n = 8)。头盔NIV组患者无创通气的时间明显增加 (28 vs .12.5, P < .001)。第90天时,头盔NIV组15名(34.1%)患者死亡,面罩NIV组22名(56.4%)患者死亡。不良事件包括,每组各有3名患者出现接触式皮肤溃疡。
总而言之,对于ARDS患者来说,头盔式NIV治疗可显著降低气管插管率。此外,头盔NIV组患者90天死亡率也显著降低。(文章详见——JAMA:头盔式无创通气可显著降低ARDS患者的气管插管率)

【4】腹部手术后发生低氧性呼吸衰竭的患者使用无创通气更能减少气管插管的风险
目前为止,对于无创性机械通气(NIV)是否可减少腹部手术后发生低氧性急性呼吸衰竭的患者有创机械通气的使用率尚无定论。本研究旨在评估无创通气是否可改善腹部手术后发生低氧性急性呼吸衰竭患者的结局。
采用多中心随机平行对照临床试验设计,于2013年5月至2014年9月在法国的20个重症监护病房进行了此项研究,共纳入了293例(平均年龄为63.4岁,224名男性)曾接受腹部手术且在术后7天内发生低氧性呼吸衰竭的患者。
将患者随机分配到标准氧疗组(n = 145,15 L/min以维持SpO2 ≥94%)或通过面罩进行的NIV治疗组(n = 148,吸气压力支持水平,5-15厘米H2O;呼吸末正压,5-10厘米H2O;滴定法测量吸入氧分数以维持SpO2≥94%)。
结果,随机化分组后7天内,包括意向治疗分析,148名NIV组患者49 名(33.1%)接受了气管插管, 145名标准治疗组66名(45.5%)患者接受了气管插管治疗。与标准氧治疗相比,非侵入性通气可明显增加无创通气的时间,且较少的患者出现了健康护理相关的感染。在第90天时,NIV组共有22名(14.9%)患者死亡,标准氧疗组共有31名患者死亡。在气体交换上两组无明显差异。
总而言之,该研究结果表明腹部手术后发生低氧性呼吸衰竭的患者,使用NIV较标准氧疗更能减少气管插管的风险。这些研究结果支持对这些患者应用NIV设置。(文章详见——JAMA:腹部手术后发生低氧性呼吸衰竭的患者使用无创通气更能减少气管插管的风险)
【5】急性呼衰,无创通气真的有效?
无创通气被推荐用于降低急性低氧性呼吸衰竭病人的死亡率,但其有效率尚不清楚。本研究旨在探究早期无创通气是否可以提高免疫力低下的急性低氧性呼吸衰竭病人的生存率。
研究设计、研究对象:研究人员于2013年8月12日至2015年1月2日之间,在法国和比利时的28个ICU的374个十分严重的病人中进行了这个多中心随机试验,其中317人(84.7%)在接受血液恶性肿瘤或者实体肿瘤的治疗。患者被随机分为无创通气组(191人)和单纯氧疗组(183人)。
结果,在随机的情况下,无创通气组中位氧流量是9L/min(四分位点内距5-15),氧疗组也是9L/min(四分位点内距5-15)。无创通气组的所有病人在入组后立刻开始无创通气,第二天有46例死亡(24.1%),氧疗组有50例死亡(27.3%)。共有155例病人(41.4%)发生氧合衰竭,73例(38.2%)在无创通气组,82例(44.8%)在氧疗组。ICU获得性感染、住院时长和机械通气时长两组无明显差异。
结论:对于收入ICU的免疫力低下的急性低氧性呼吸衰竭病人,早期无创通气和单纯氧疗相比未能降低28天死亡率。但因研究有局限性,还需要更多更深入的研究以确定最终结论。(文章详见——JAMA:急性呼衰,无创通气真的有效?)

本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












ards用无创可以吗?
87
#无创通气#
59
继续关注
84
继续学习
0
这个学习了,争议
75
谢谢,学习知识
89
学习了,非常有帮助,谢谢。
60
适合就好
52
verygood!p
35
讲的真好,学习了
64