JAHA:糖尿病与心房颤动表型以及心脏和神经系统合并症的关联
2021-11-11 MedSci原创 MedSci原创
与非糖尿病患者相比,伴有糖尿病的AF患者较少感知到AF症状,但生活质量较差,心脏和神经系统合并症更多。
糖尿病是心房颤动(AF)的主要危险因素,将糖尿病与AF联系起来的潜在机制涉及心房的电、结构和自主神经重构。然而,目前尚不清楚伴有和不伴有糖尿病的AF患者个体AF表型和相关合并症是否存在差异。
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,该研究旨在调查AF患者糖尿病与AF表型以及心脏和神经系统合并症之间的关联。
改研究的主要结局是AF表型的参数,包括AF类型、AF症状和生活质量(由欧洲生活质量5维度问卷[EQ-5D]评估),该研究的次要结局是心脏(即高血压、心肌梗死和心力衰竭病史)和神经系统(即卒中和认知障碍病史)合并症。研究人员使用Logistic回归和线性回归评估糖尿病与这些结局之间的横断面关联,并根据年龄、性别和心血管危险因素进行调整。
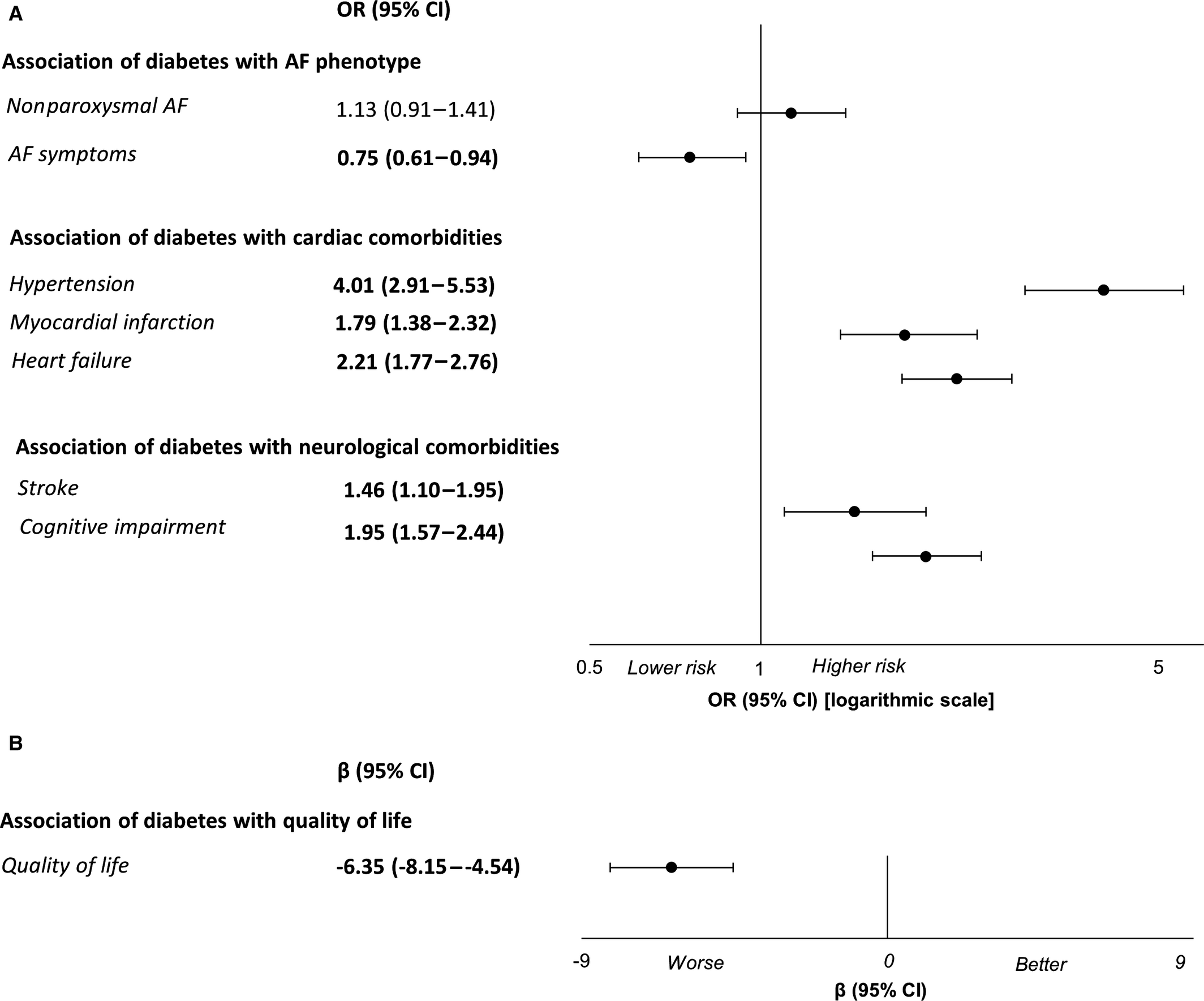
研究人员纳入了2411名AF患者(27.4%为女性;中位年龄为73.6岁)。糖尿病与非阵发性AF无关(比值比[OR]为1.01;95%CI为0.81-1.27)。与没有糖尿病的患者相比,糖尿病患者较少感知到AF症状(OR为0.74;95%CI为0.59-0.92),但生活质量更差(β=-4.54;95%CI为-6.40至-2.68)。糖尿病患者更可能患有心脏疾病(高血压[OR为3.04;95%CI为2.19-4.22]、心肌梗死[OR为1.55;95%CI为1.18-2.03]、心力衰竭[OR为1.99;95%CI为1.57-2.51])和神经系统(卒中[OR为1.39,95%CI为1.03-1.87],认知障碍[OR为1.75,95%CI为1.39-2.21])合并症。
由此可见,与非糖尿病患者相比,伴有糖尿病的AF患者较少感知到AF症状,但生活质量较差,心脏和神经系统合并症更多。
原始出处:
Arjola Bano,et al.Association of Diabetes With Atrial Fibrillation Phenotype and Cardiac and Neurological Comorbidities: Insights From the Swiss‐AF Study.JAHA.2021.https://www.ahajournals.org/doi/full/10.1161/JAHA.121.021800
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#合并症#
68
#AHA#
68
#神经系统#
62
#表型#
0
#心房#
83
已拜读,受益匪浅。
98
已拜读,受益匪浅。
86
,学习学习
79
学习一下
102
胆汁酸是胆汁的重要组成成分,是人
88