李太生教授团队:高剂量静脉注射免疫球蛋白——COVID-19重症患者安全有效的普适疗法
2020-05-04 李太生 北京协和医院
作者:中国医学科学院 北京协和医学院 北京协和医院 林铃 曹玮 李太生
作者:中国医学科学院 北京协和医学院 北京协和医院 林铃 曹玮 李太生*
2019年12月,严重急性呼吸道综合征冠状病毒2型(SARS-CoV-2)爆发,传播迅速。截至目前为止,虽有许多经验性治疗方案,包括现有的和新的抗病毒药物、类固醇和中药等,但对于严重SARS-CoV-2肺炎的最佳治疗策略仍不清楚。
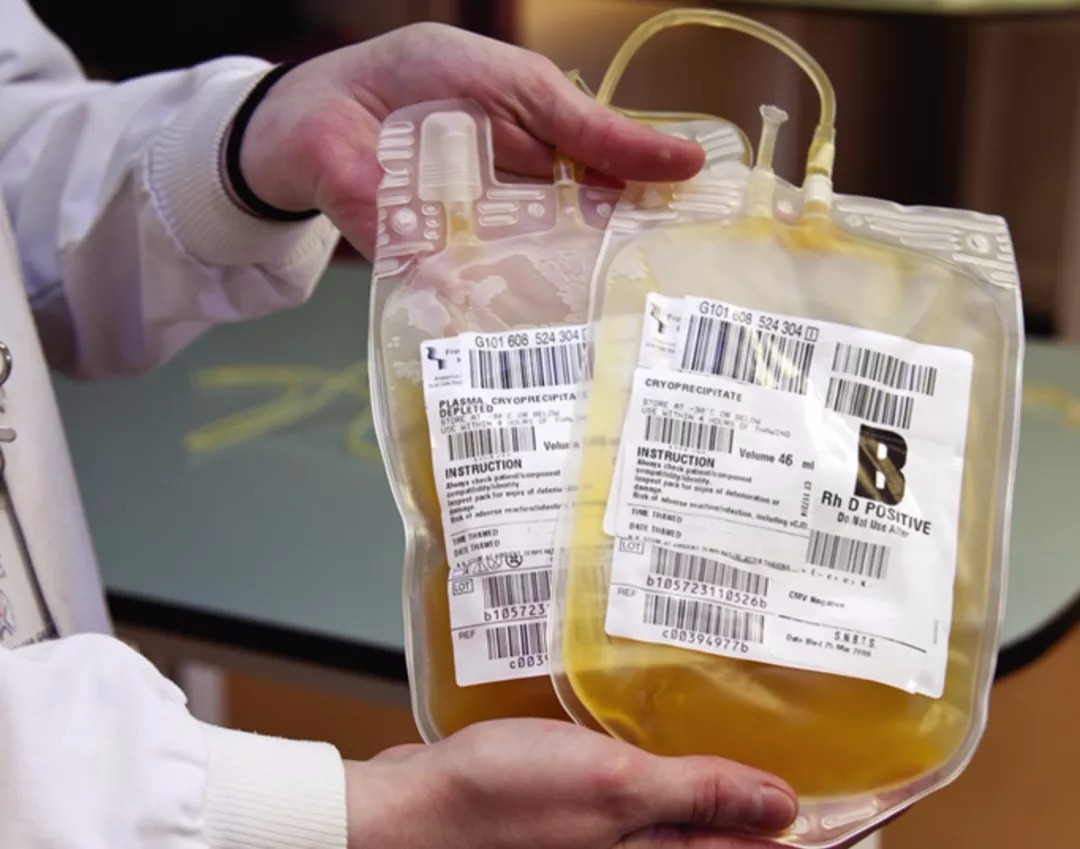
2020年3月下旬,Open Forum Infectious Diseases发布了李太生及阮连国团队对于2019冠状病毒疾病(COVID-2019)重症患者的一篇简短报告《高剂量静脉注射免疫球蛋白可作为新冠病毒病(COVID-19)病情恶化患者的一种治疗选择》(High-Dose Intravenous Immunoglobulin as a Therapeutic Option for Deteriorating Patients With Coronavirus Disease 2019)。
在此篇案例报告中,李太生等人报告了3例接受大剂量静脉注射免疫球蛋白(IVIg)为主要治疗的重症SARS-CoV-2感染的肺炎患者,经过治疗,3例患者无论从临床还是影像学表现上都有很好的改善。提示基于IVIg潜在的免疫调节机制和被动免疫的功能,临床重症、危重症患者早期给予高剂量IVIg可能是有益的。
病例介绍
病例1
56岁男性,发热、咽痛2日,最高体温(Tmax) 38.2 ℃,普通抗病毒及抗菌药物治疗无效。2020年1月22日入院CT提示右侧弥散性间质斑片影及胸膜增厚,鼻咽拭子检测SARS-CoV-2阳性。
患者于入院第5天出现呼吸道症状加重,血氧饱和度91%,炎症指标升高明显,CT示肺部病变加重。由普通型快速进展为重型。
入院第7天予IVIg 25 g,连续5天输注。使用当日,患者体温正常,5天后情况好转,血氧饱和度恢复至98%,炎症指标降低,影像学好转,核酸检测两次阴性,于2月5日出院。
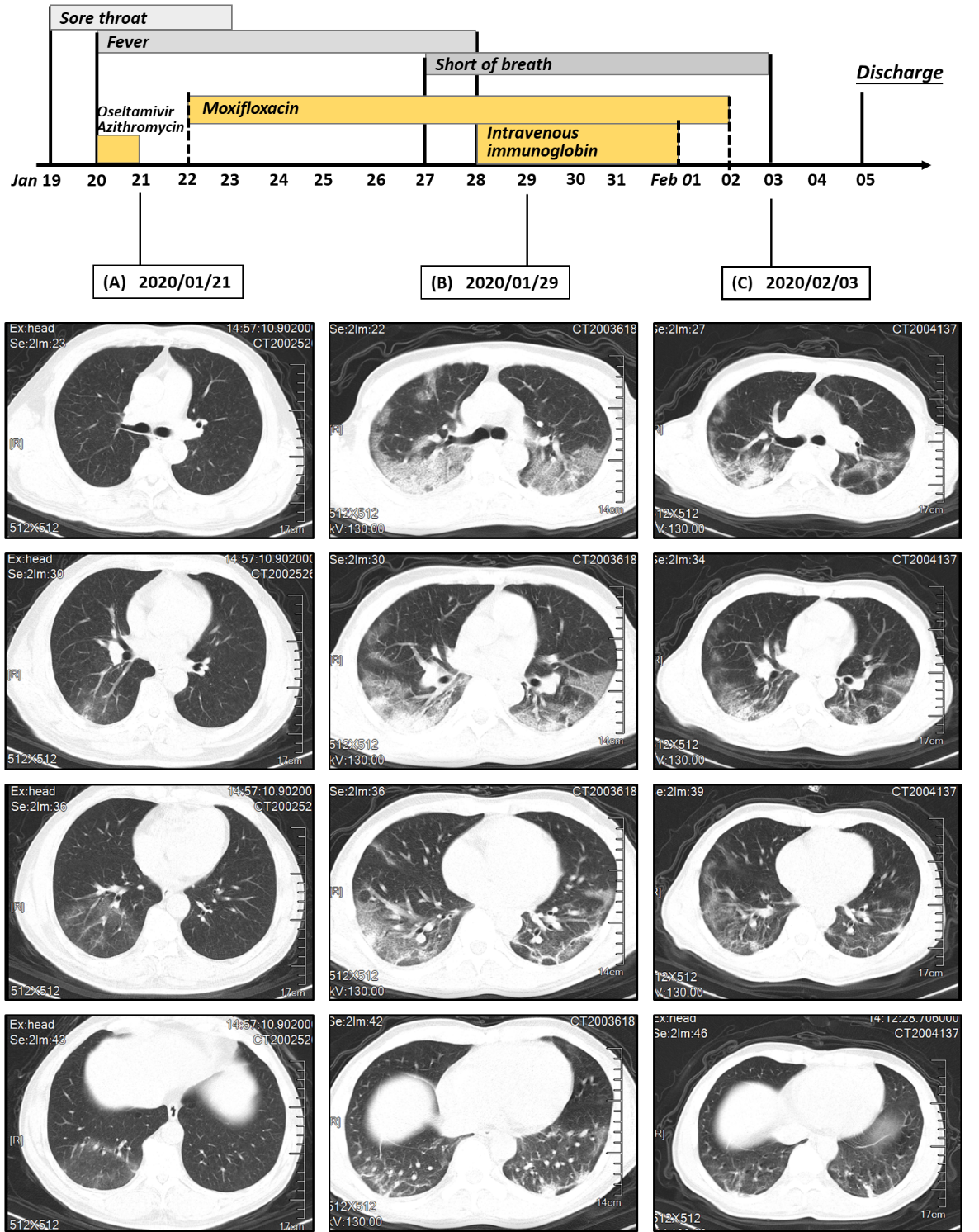
图1 患者1自2020年1月19日至2月5日的症状,CT平扫和治疗
病例2
34岁男性,发热、干咳10日,Tmax 38.5 ℃,合并高血压病病史。因呼吸急促就诊,查鼻咽拭子SARS-CoV-2阳性。2020年1月29日入院后血氧饱和度90%,实验室检查示血小板减少,肌酸激酶(CK)、肌红蛋白(Myo)升高,CT示双侧多发浸润及浑浊,评估为重型。立即予IVIg,25 g连续5日输注。使用第2日,患者呼吸困难症状逐渐改善,2月3日复查CT炎症明显吸收,核酸检测两次阴性,于2月5日出院。
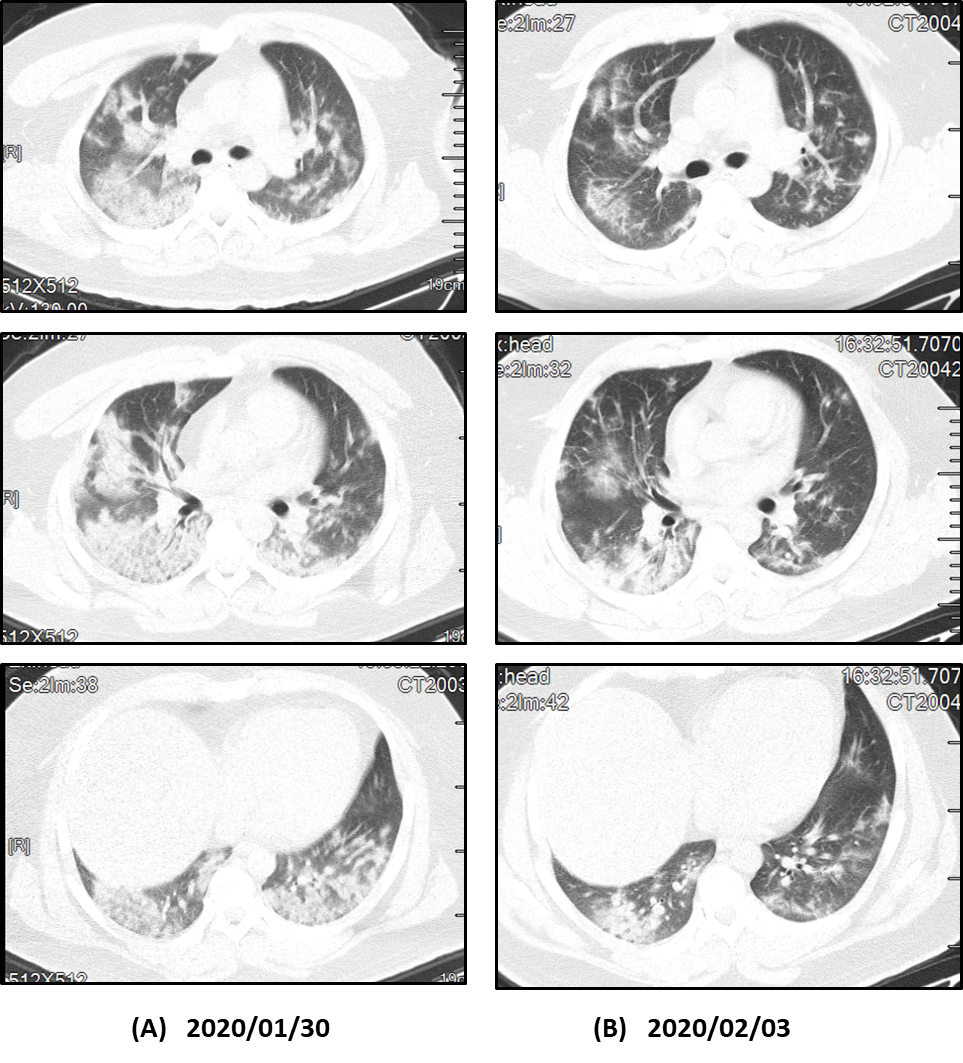
图2.患者2 IVIG治疗前后CT平扫
病例3
35岁女性,低热,咳嗽,1月20日 Tmax 37.3 ℃。鼻咽拭子SARS-CoV-2阳性,诊断为COVID-2019。
1月29日,患者病情加重,出现呼吸短促,血氧饱和度降低,淋巴细胞进一步减少,炎症指标持续升高,CT见病变范围增大。由普通型快速进展为重型。予IVIg,25 g连续5日输注,同时予甲泼尼龙40 mg/d×3 d。使用第一天,患者体温正常,两天后血氧饱和度恢复,症状改善。复查胸CT好转,核酸检测两次阴性,于2月9日出院。
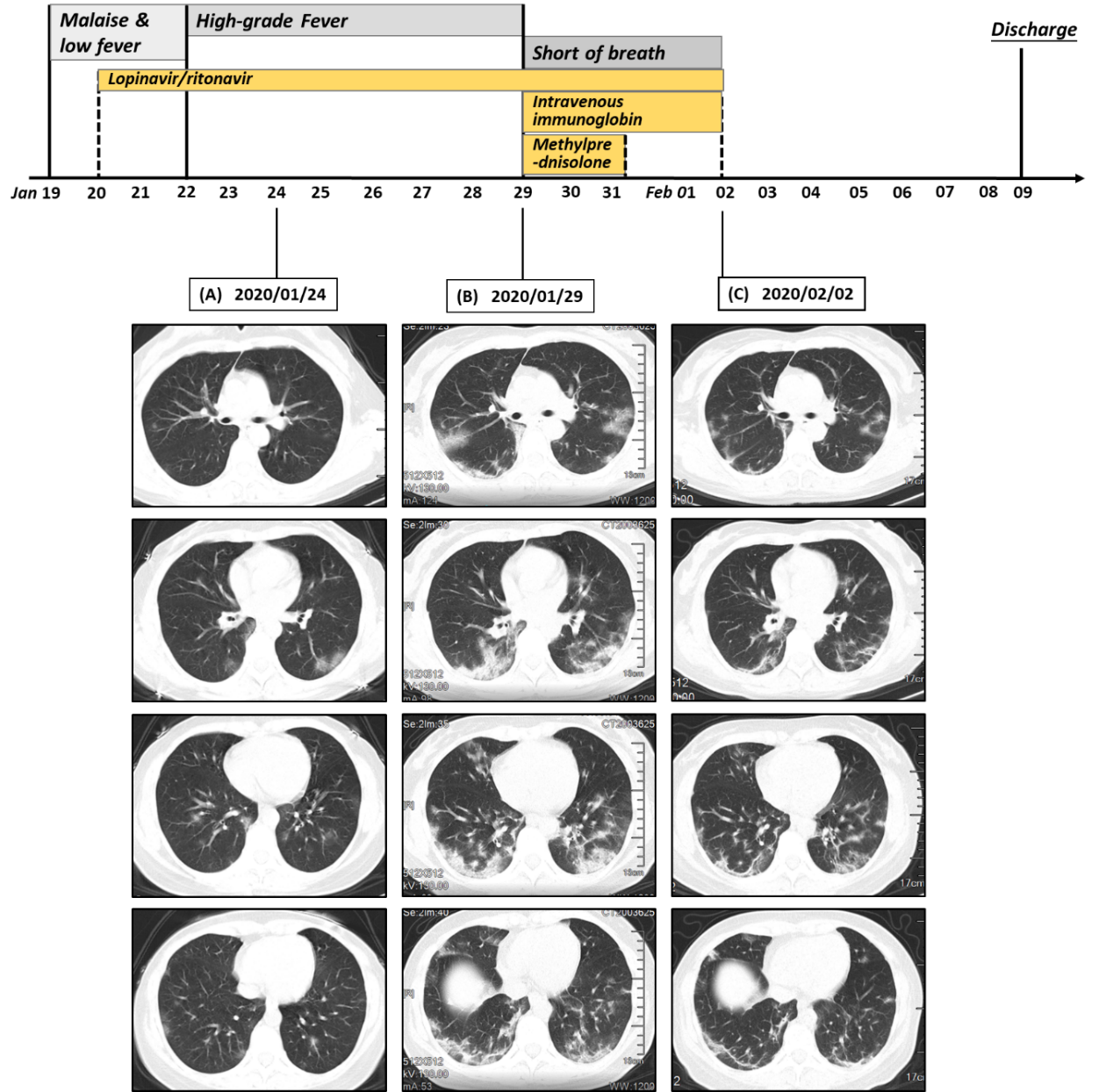
图3 患者3自2020年1月19日至2月9日的症状,CT平扫和治疗
病例总结与分析
根据患者以轻微或中度的非特异性症状发病,结合患者CT影像学显示病变从肺外带开始,提示病毒感染之后可出现病毒血症阶段,当病毒引起针对器官和组织的继发性损伤发生时,包括肺部、心脏、胃肠道等均会出现损伤,甚至可以引起全身的炎症因子风暴。实验室检查主要提示为炎症指标升高,淋巴细胞进行性减少。
基于以上观察,williamhill asia 提出了在疾病发展即将或刚开始进入加速阶段的时候,有效抑制炎症的级联反应,可以使患者免于致命的免疫介导的损伤。
因此,发病早期给予重症患者每天每公斤体重0.3~0.5 g的高剂量IVIg作为一种有效和安全的免疫调节剂,或可为一种治疗选择。
(本文经李太生教授授权发布,转载请申请)
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言















#患者安全#
80
#静脉#
52
#球蛋白#
61
#高剂量#
65
#免疫球蛋白#
58
#重症患者#
59
#静脉注射#
58
#李太生#
53